6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ff84ee040000008802000001000700
6go6ckt5b5idvals|277
6go6ckt5b5idcol1|ID
6go6ckt5b5|2000F757Tab_Articles|Fulltext
Introduction
Gallbladder perforation is a rare but serious complication of cholecystitis. It rarely presents as abdominal wall abscess, necrotizing fasciitis or cholecystocutaneous fistula due to delay in diagnosis. Gallbladder perforation is generally an operative diagnosis, but a high index of suspicion and diagnostic modalities such as ultrasonography and CT scan can aid in diagnosing gallbladder perforation preoperatively. Early diagnosis and surgical interventions are the factors to decrease morbidity and mortality in the management of gallbladder perforation with complications.
Case Report
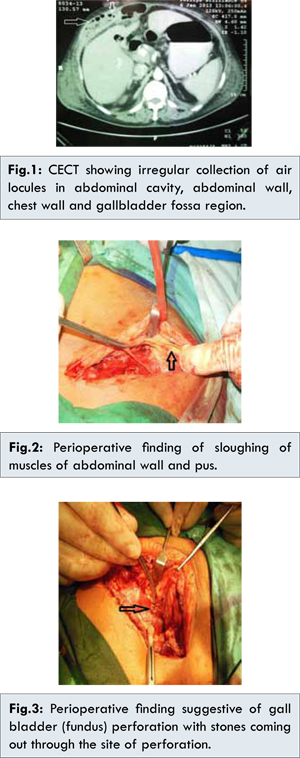
An 80 year old obese female presented with 10 days history of right upper quadrant abdominal pain without any history of fever and vomiting. Her vitals at admission were pulse rate 96/min, BP 140/90 mmHg. Abdominal examination showed tenderness in epigastrium, right hypochondrium and right lumbar region and diffuse subcutaneous crackling was present from right lower part of chest to the level of umbilicus without any signs of cellulitis. Systemic examination of chest revealed bilateral crepitations and rhonchi. Laboratory studies showed white cell count 22,900/cu.mm and all other investigations were within normal limits. Initial sonographic evaluation of abdomen revealed hepatomegaly, cholelithiasis with thick walled gallbladder suggestive of acute cholecystitis with presence of gas in anterior abdominal wall limiting scan. CECT abdomen [Fig.1] revealed irregular collection with internal air locules in anterior part of upper abdominal cavity extending into the anterior abdominal wall and right lower part chest wall as well as in gall bladder fossa region with nonseparate visualization of the gall bladder suggestive of gall bladder rupture with minimal pelvic fluid. The patient was operated through right subcostal incision and just after opening of anterior abdominal wall sloughing of muscle [Fig.2] with necrotic tissue from lower part of chest to the level of umbilicus was present. Gall bladder was perforated at fundus with multiple stones [Fig.3]and it was communicating with subcutaneous tissue. Cholecystectomy and debridement of necrotic area was done. Postoperatively patient developed shock and multiple organ dysfunction syndrome (MODS)secondary to Klebsiella sepsis and expired two days later.
Discussion
Perforation of gallbladder is unusual complication and the incidence of the gallbladder perforation is reported to vary from 3% to 10% [
1,
2]. This type of presentation as chest wall cellulitis is previously not reported. There are various sites of perforation of gall bladder stated in literature like the junction of cystic and common hepatic duct, common hepatic duct and junction of cystic duct and gallbladder and lastly gallbladder itself, as in our case the fundus [
3,
4].
Ultrasound is the initial imaging modality of choice for the evaluation of acute gallbladder disorders. However, in cases of complication of acute cholecystitis like emphysematous cholecystitis, hemorrhagic cholecystitis, and gallbladder perforation; ultrasound is of limited value where role of CT scan becomes more important [
5]. The hole sign (visualization of defect in the gall bladder) is the only reliable sign of gall bladder perforation on ultrasound [
6]. In our patient, ultrasound failed to provide information about gall bladder perforation except thick gall bladder and multiple stones. Sood et al showed a marginally higher rate of detection of gallbladder wall defects on CT than with ultrasonography [
6,
7]. In our patient, diagnosis was made by CT abdomen and confirmed during surgery. The best form of management for perforation gall bladder is prompt surgery as delay in intervention leads to substantial increase in both mortality and morbidity.
Conclusion
Abdominal wall abscess is an infrequent cause of potentially life threatening gallbladder perforation. This can begin in a subtle fashion which, if undiagnosed for a prolonged period of time, sometimes evolves into life threatening complication. CECT abdomen remains the investigation of choice. The critical management issue is diagnosing and treating acute cholecystitis promptly, before irreversible damage and loss of tissue integrity occurs.
References
- Rosyln JB, Usuttil RW. Perforation of gallbladder: A frequently mismanaged condition. Am J Surg. 1979;137:307-312
- Simmons TC, Miller C, Weaver R. Spontaneous gallbladder perforation. Am Surg. 1989;55: 311-313.
- Beck HI, Jensen PO. Non-traumatic intrahepatic rupture of biliary tree. Acta Chir Scand. 1981;147:297.
- Isch JH, Finneran JC, Nahrwold DL. Perforation of the gall bladder. Am J Gastroenterol. 1971;55:451-458.
- Bennett GL, Balthazar EJ. Ultrasound and CT evaluation of emergent gallbladder pathology.Radiol Clin North Am. 2003;41(6):1203-1216.
- Sood BP, Kalra N, Gupta S, Sidhu R, Gulat M, Khandelwal N, et al. Role of sonography in the diagnosis of gallbladder perforation. J Clin Ultrasound. 2002;30:270-274.
- Parathithasan N, Naqash N. Acute Presentation of Gallbladder Carcinosarcoma and Management. Journal of Case Reports. 2013;3(2):370-375.