Introduction
Gastrointestinal complications of enteric fever are intestinal haemorrhage and perforation, acute pancreatitis, hepatic abscess, acute cholecystitis, splenic rupture and hepatitis [1]. Initial gastrointestinal presentation as pancreatitis is an extremely rare manifestation of enteric fever [2]. This atypical presentation has to be borne in mind in dealing with a case of fever with abdominal pain in an endemic country like India especially if additional suggestions are present.
Case Report
A 27 year old non-diabetic, non-hypertensive male patient was admitted with the chief complaints of fever and pain abdomen for last 8 days. Fever was high grade, intermittent and associated with chills and rigor. Abdominal pain was localised to epigastric region with occasional radiation to the back, constant and boring in nature, increasing in supine position and responded partially to medications. He also had loose stools and vomiting but no passage of blood in stool. He developed progressively increasing breathlessness over the last 2 days. There was no history of cough, chest pain, palpitation, sweating, giddiness, decreased urine output, swelling of legs or any bleeding manifestations. The patient was non-alcoholic and non-smoker. He did not have any history of any chemotherapeutic drug or antiretroviral drug intake.
On general examination, patient was conscious, alert and oriented; dehydration was present. He was febrile with axillary temperature 39oC. He also had mild pallor and icterus, and was tachypneic with a respiratory rate of 36/min and 91% oxygen saturation in room air. Blood pressure was 104/66 mmHg with no significant postural drop. On systemic examination, decreased breath sounds and crepitations over both the bases of the lungs were noted along with generalised, diffuse tenderness in abdomen with sluggish bowel sounds. Examination of the other systems did not reveal any notable abnormalities.
Investigations revealed WBC count: 3100/cumm, platelet count: 90,000/cumm, haemoglobin: 8.4 g/dL and an ESR of 48 mm/1st hour. Peripheral smear showed normocytic normochromic anemia and left sided shift of leukocytes and pancytopenia. Acid blood gas analysis showed evidence of type 1 respiratory failure. Serum electrolytes revealed Na+: 134 meq/L, K+: 3.2 meq/L and Ca+2: 8.2 mg/dL. Lipid profile (including triglyceride) was normal. Liver function tests showed direct hyperbilirubinemia (conjugated bilirubin: 1.8 mg/dL, unconjugated bilirubin: 1.2 mg/dL); elevated transaminases as well as alkaline phosphatase (AST: 67 U/L; ALT: 77 U/L; Alkaline phosphatase: 325 U/L); normal albumin and globulin levels. Serum amylase and lipase were significantly elevated: amylase-689 U/L (normal 30-120 U/L); lipase-532 U/L (normal 10-140 U/L). Serum lactate dehydrogenase (LDH) levels was also elevated: 556 U/L (normal 105-220 U/L). Serum creatinine was 1.6 mg/dL; urea: 70 mg/dL (suggesting presence of pre-renal failure). Serum creatine phosphokinase (CPK) was normal. Routine urine analysis showed trace proteinuria.
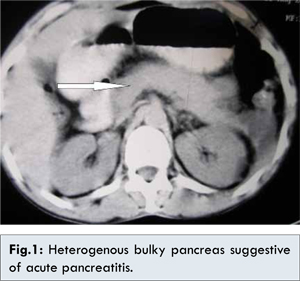
Ultrasonography (USG) abdomen revealed mild hepato-splenomegaly with mild ascites. A notable finding was the presence of edematous, heterogenous appearing head and body of pancreas with strong possibility of acute pancreatitis. No gallstones or biliary tract abnormalities were noted on USG. Contrast enhanced Computed Tomography (CECT) abdomen showed presence of severe acute pancreatitis [Fig.1]. Chest X-ray showed bilateral trace pleural effusion. Pleural fluid study was transudative in nature. Urine culture, stool routine and culture showed no growth. However, blood culture grew Salmonella typhi which was sensitive to third generation cephalosporins. A final diagnosis of enteric fever complicated by acute pancreatitis with evidence of acute hepatitis, prerenal failure and type 1 respiratory failure was made. The patient was started on adequate intravenous fluids, ceftriaxone (based on the culture-sensitivity pattern). The patient’s general condition improved and he was discharged in a stable condition on 17th day of admission.
Patients with enteric fever may present with abdominal pain and the causes for abdominal pain in a patient with enteric fever are intestinal haemorrhage and perforation, acute cholecystitis, typhoid hepatitis, hepatic abscess, splenic rupture and acute pancreatitis [1,2]. Enteric fever masquerading as acute pancreatitis is a rare entity [3]. The abnormalities of pancreas that are associated with typhoid fever may include simple biochemical abnormalities such as hyperamylasemia to acute pancreatitis, pancreatic abscess, chronic pancreatitis, pancreatic pseudocyst requiring surgery [4,5].
Retrospective studies have reported a frequency of hyperamylasemia of 50% and a frequency of clinical pancreatitis ranging from 28 to 62% in patients with Salmonella infection [6]. Few case reports have highlighted the association of acute pancreatitis and other pancreatic complications with Salmonella infections. Two cases of acute pancreatitis by Salmonella typhi were reported by Koshi [1]. One of these cases required distal pancreatectomy while the other required only drainage of pseudocyst. The first case of pancreatic abscess due to Salmonella typhimurium was reported by Strand and Sanders [7]. The notable feature was that the case had associated gallstones and chronic cholecystitis. The index patient here had normal gall bladder and biliary tract. Khan et al reported a case of enteric fever complicated by acute pancreatitis, acute renal failure and rhabdomyolysis [8]. In our case, only prerenal failure and not renal failure was noted and no evidence of rhabdomyolysis was present.
Localized Salmonella infection of the pancreas isusually the result of Salmonella bacteraemia causedby Salmonella choleraesuis but may also occur after gastroenteritis by S. typhimurium and enteric fever by Salmonella typhi [9]. Once pancreatitis develops, it may form a pancreatic abscess. Pancreatic pseudocyst may occasionally be infected by Salmonella typhi [2]. Salmonella typhi is known to localize in injured or damaged tissue or insites of malignancy [3]. Kune and Coster reported a case of pancreatic abscess due to Salmonella typhi who had gallstones; the organism was isolated from the necrotic pancreatic tissue [10].
Mechanism of pancreatitis in enteric fever is not exactly known. Typhoid pancreatitis could represent the effect of the direct pancreatic localisation of bacteria which could happen by haematogenous route, lymphatic route and transmural migration, via the biliary duct system and from the duodenum via the main pancreatic duct. This may occur, especially in patients with predisposing conditions to biliary stasis, such as cholelithiasis, choledocholithiasis, and biliary duct abnormalities [11], but our patient had no such predisposing conditions. The mechanisms may also be toxin induced or immune mediated pancreatitis [12,13]. Isolated hyperamylasemia and hyperlipasemia without evidence of pancreatic involvement could also be the result of a reduced excretion due to either impaired renal or liver function which is common in Salmonella infections. Concomitant hepatitis (as in our case) and renal failure may contribute to cause abnormally elevated levels of amylase and lipase than what would be expected by isolated pancreatitis alone [14]. Gnadinger MP et al suggested that the excess of hyperamylasemia seen in Salmonella infections may be due to intestinal inflammation leading to abnormally increased absorption of macromolecules like amylase; he demonstrated an increased intestinal permeability for oral 51Cr-EDTA in two patients with elevated amylase serum levels in the course of entero-invasive salmonellosis. However, other studies have failed to reproduce this finding [15].
Treatment includes aggressive management of both typhoid fever and acute pancreatitis [3]. Treatment with anti-secretory drugs, by reducing the gastric killing of ingested organisms, has been shown to represent a risk factor for severity and mortality, so its administration is strongly discouraged [16].
Conclusion
This case highlights the importance of keeping in mind the possibility of development of acute pancreatitis in a case of enteric fever as appropriate diagnosis and treatment might lead to complete resolution of the potentially fatal condition. Salmonella infection must be considered in cases of non-alcoholic or non-lithiasic pancreatitis.
References
- Koshi G. Uncommon manifestations of salmonella infections. Indian Journal of Medical Research. 1976;64(2):314-321.
- Bhan MK, Bahl R, Bhatnagar S. Typhoid and paratyphoid fever. Lancet. 2005;366:749-762.
- Hermans P, Gerard M, van Laethem Y, de Wit S, Clumeck N. Pancreatic disturbances and typhoid fever. Scandinavian Journal of Infectious Diseases. 1991;23(2):201-205.
- Renner F, Nimeth C, Demmelbauer N. High frequency of concomitant pancreatitis in Salmonella enteritis. Lancet. 1991;337(8757):1611.
- Kadappu KK, Rao PV, Srinivas N, Shastry BA. Pancreatitis in enteric fever. Indian Journal of Gastroenterology. 2002;21(1):32-33.
- Renner F, Nimeth C, Demmelbauer N. High frequency of concomitant pancreatitis in Salmonella enteritis. Lancet 1991;337:1611.
- Strand CL, Sanders SL. Salmonella typhimurium pancreatic abscess - report of a case. Am Surg. 1978, 44:174-176.
- Khan FH, Al-Ani A, AliHA. Typhoid rhabdo-myolysis with acute renal failure and acute pancreatitis: a case report and review of the literature.Int J Infect Dis. 2009;13(5):e282-e285.
- Cohen JI, Bartlett, JA, Correy GR. Extraintestinal manifestations of salmonella infection. Medicine. 1987;66:349-388.
- Kune, GA, Coster D. Typhoid pancreatic abscess. Med J Aust. 1972;1:417-418.
- Hearne SE, Whigham TE, Brady CE. Pancreatitis and typhoid fever. Am J Med. 1989;86:471–473.
- Arendt T. Bile-induced acute pancreatitis in cats.Roles of bile, bacteria, and pancreatic duct pressure. Dig Dis Sci. 1993;38(1):39-44.
- Schmid SW, Uhl W, Friess H, Malfertheiner P, Büchler MW. The role of infection in acute pancreatitis. Gut. 1999;45(2):311-316.
- Pezzilli R, Andreone P, Morselli-Labate AM, Sama C, Billi P, Cursaro C, et al. Serum pancreatic enzyme concentrations in chronic viral liver diseases. Dig Dis Sci.1999;44:350-355.
- Gnadinger MP, Eigenmann F, Bekier A, Galeazzi RL. Pseudopancreatitis in entero-invasive salmonellosis. Schweiz Med Wochenschr. 1993;123:1482-1486.
- Neal K, Briji SO, Slack RC, Hawkey CJ, Logan RF. Recent treatment with H2 antagonists and antibiotics and gastric surgery as risk factors for Salmonella infection. BMJ. 1994;308:176.