6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ffe835350000006a07000001000700
6go6ckt5b5idvals|3089
6go6ckt5b5|2000F757Tab_Articles|Fulltext
Introduction
Gall stone ileus (GSI) is occlusion of the intestinal lumen as a result of one or more gallstones [
1-
2] which generally pass through enterobiliary fistula. GSI is responsible for only 1-4% of all cases of mechanical bowel obstruction. The symptoms and signs of gallstone ileus are mostly non-specific. This entity has been observed with a higher frequency among the elderly females, the majority of which have concomitant medical illness. The mortality rates in patients with gall stone ileus are usually high, ranges between 12 and 27% [
3], as it occurs in elderly patients. The optimal management of acute gall stone ileus is controversial [
4], but enterotomy with stone extraction remains the most common surgical method because it has low incidence of complications.
Case Report
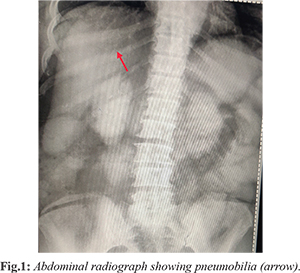
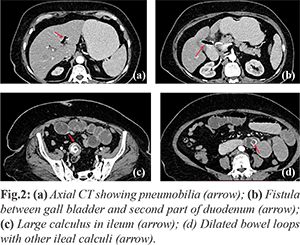
A 60-year-old female was referred to our department with multiple episodes of intermittent vomiting and abdominal pain in epigastric region for 3 days. This patient had similar episode of pain 1 yr back. She had been treated in another hospital with intravenous fluids and antibiotics. Upon examination, her abdomen was moderately distended, tympanic and high-pitched bowel sounds were audible. Rectal examination was normal. Blood tests revealed an elevated total leukocyte count (14.4×109 cells/L) and unremarkable liver function test values. Plain radiographs of the abdomen showed air in the biliary tree [Fig.1]. Ultrasound (USG) revealed cholelithiasis and pneumobilia suggesting possibility of fistulous communication between gallbladder and second part of duodenum along with small bowel loop obstruction. Contrast enhanced computed tomography (CECT) revealed pneumobilia, contracted and edematous gall bladder with evidence of fistula between gall bladder and second part of duodenum with peri-cholecystic inflammation. A calculus measuring 2.4 cm was noted at ileum causing small bowel obstruction with dilatation of duodenal and jejunal loops. Four non-obstructing calculi were also noted in dilated small bowel loop segments proximal to largest calculus [Fig.2a-d]. CT findings were consistent with gall stone ileus and showed all the components of Rigler’s triad i.e pneumobilia, small bowel obstruction and ectopic calcified stone.
The patient underwent an exploratory laparotomy and presence of a wide fistula from the gallbladder to the second part of the duodenum was confirmed. Gall stone was seen in distal ileum with dilated proximal jejunal and illeal loops [Fig.3]. Milking of stone was done towards proximal ileum ~10 cm from the impacted site. Longitudinal incision over anti-mesenteric border was given and the stone was retrieved. Decompression of the dilated loops was done and multiple other calculi were retrieved too and enterotomy repaired in two layers. The patient had an uneventful post-operative course and was discharged home on post-operative day 6.
Discussion
Women are more prone to GSI, and the ratio of females to males is 3.5 to 1. The gallstone may enter the intestine through a fistula and it must be = 2-2.5 cm in diameter to cause obstruction [
5]. There are six factors known to cause a fistula: foreign body, radiation, inflammation, epithelialization, neoplasia, and distal obstruction. Impaction of the stone can occur in any part of the bowel, but it occurs most frequently in the terminal ileum and the ileocecal valve because of their narrow lumen and potentially less active peristalsis. Once a gallstone has impacted within the small bowel and caused ileus, it rarely passes out spontaneously through the intestine [
6]. Symptoms are typically non-specific, presenting with nausea, vomiting, abdominal distension and pain. In the past, confirming the diagnosis was difficult, but the advent of CT and magnetic resonance imaging (MRI), Rigler’s triad can be easily demonstrated [
7].
Classical findings on plain abdominal radiography include pneumobilia, intestinal obstruction, an aberrantly located gallstone; and change in location of a previously observed stone [
8]. However, sometimes non-detection of gall stones and pneumobilia on X-ray results in delayed diagnosis. Therefore, CECT abdomen remains the most helpful diagnostic tool for gall stone ileus as it is highly sensitive, specific, and accurate [
9]. The findings of CT (Rigler’s triad) include obstruction of the small intestine, ectopic gallstones, pneumobilia. The decision regarding conservative management can be done on the basis of information obtained from CT such as the site of obstruction, migration of the gallstone and size of the impacted gallstone, as stones less than 2.5 cm usually pass through without getting impacted. In our case suspicion of gall stone ileus on USG was confirmed on CT and surgical intervention in the form of enterotomy and stone retrieval resulted in reduced morbidity of the patient.
Surgical management of GI is controversial and includes: (i) enterotomy with stone extraction alone; (ii) enterotomy, stone extraction, cholecystectomy and fistula closure; (iii) bowel resection alone; and (iv) bowel resection with fistula closure [
10]. Enterotomy with stone extraction alone remains the most common surgical method because of its low incidence of complications. Spontaneous closure of the fistulous tract is observed in >50% of cases. In literature review, fistula closure if conducted, urgently or as an emergency during the initial procedure, is independently associated with a higher prevalence of mortality than enterotomy and stone extraction alone. If the gallbladder is preserved at the initial procedure, delayed cholecystectomy must be considered. Sometimes patients who had undergone enterolithotomy alone go on to develop biliary symptoms, with the risk of patent fistula reflux and resulting biliary malignancy. Bowel resection is sometimes necessary, particularly in the presence of a perforation.
Conclusion
Disproportionate symptoms and signs of small bowel obstruction in a patient with gall stone disease should alert the surgeon to suspect GSI and investigate with combined diagnostic imaging modalities (mainly abdominal plain film and CT scan) as soon as possible. The presence of Rigler’s triad in imaging should prompt the surgeon to relieve intestinal obstruction quickly, to minimize morbidity and mortality. Literature review generally supports the employment of enterolithotomy in high-risk patients and reserving cholecystectomy and resection of the fistula for less co-morbid patients with feasible anatomy.
Contributors: MK: manuscript editing, imaging; NS: manuscript writing, imaging. MK will act as a study guarantor. Both authors approved the final version of this manuscript and are responsible for all aspects of this study.
Funding: None; Competing interests: None stated.
References
- Chatterjee S, Chaudhuri T, Ghosh G, Ganguly A. Gallstone ileus-an atypical presentation and unusual location. Int J Surg. 2008;6:e55-e56.
- Chou JW, Hsu CH, Liao KF, Lai HC, Cheng KS, Peng CY, et al. Gallstone ileus: report of two cases and review of the literature. World J Gastroenterol. 2007;13:1295-1298.
- Reisner RM, Cohen JR. Gallstone ileus: a review of 1001 reported cases. Am Surg. 1994;60: 441-446.
- Halabi WJ, Kang CY, Ketana N, Lafaro KJ, Nguyen VQ, Stamos MJ, et al. Surgery for gallstone ileus: A nationwide comparison of trends and outcomes. Ann Surg. 2014;259(2):329-335.
- Syme RG. Management of gallstone ileus. Can J Surg. 1989;32:61-64.
- Farooq A, Memon B, Memon MA. Resolution of gallstone ileus with spontaneous evacuation of gallstone. Emergency Radiology. 2007;14:421-423.
- Gupta M, Goyal S, Singal R, Goyal R, Goyal SL, Mittal A. Gallstone ileus and jejunal perforation along with gangrenous bowel in a young patient: A case report. N Am J Med Sci. 2010;2:442-443.
- Al-Obaid O. Gallstone ileus: a forgotten rare cause of intestinal obstruction. Saudi J Gastroenterol. 2007;13:39-42.
- Yu CY, Lin CC, Shyu RY, Hsieh CB, Wu HS, Tyan YS, et al. Value of CT in the diagnosis and management of gallstone ileus. World J Gastroenterol. 2005;11:2142-2147.
- Ravikumar R, Williams JG. The operative management of gallstone ileus. Ann R Coll Surg Engl. 2010;92:279-281.