6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ffa49335000000230a000001000100
6go6ckt5b5idvals|3092
6go6ckt5b5|2000F757Tab_Articles|Fulltext
Introduction
Tracheo-bronchial tree injuries are rare, but potentially life-threatening, in both adults and children. They are well-known sequel of massive blunt or penetrating injuries of the neck or chest [
1,
2], that may occur as a rare complication of endotracheal intubation [
3-
5]. Spontaneous tracheal ruptures are extremely uncommon, and few cases have been reported in literature. We report two cases of trachea-bronchial tree injury secondary to lower respiratory tract infection and chronic obstructive pulmonary disease (COPD) with steroid use worsened secondary to intubation. Challenges of airway management and stabilisation are dealt with in these case reports.
Case Reports
Case 1
A 23-year-old female came with history of fever and cough with expectoration in the past 3 days and associated breathlessness for 1 day. Fever was moderate grade with chills not subsiding with oral medication associated with expectorant cough and dyspnea, which acutely worsened. No history of trauma or co-morbidities were present. The patient was referred from another hospital on oxygen mask with sudden onset swelling of her face and chest and both upper limbs since the last 3 hours. On arrival her pulse rate was 130/min, BP recording was 90/60 mm of Hg, RR was 44/min, room air saturation was 78% and on oxygen it was 84% and she was afebrile. General physical examination revealed extensive subcutaneous emphysema with crepitus over face, chest wall, extending to bilateral upper limbs. A possibility of trachea bronchial tree injury (TBI) was considered at this point. Anaphylaxis was another consideration but subcutaneous crepitation with sparing of lips pointed more in favour of TBI.
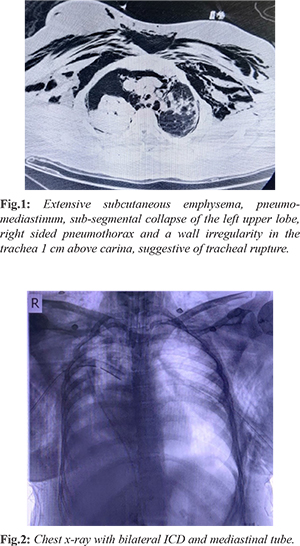
The patient was intubated under direct vision with smooth and gentle passage of the tube. Measures were ensured for anticipated difficult airway and front of neck access (FONA) team was standing by. After intubation her vitals were HR: 110/min, BP: 80/60 mm Hg, SpO2 88% on a ventilator. Bilateral inter-costal drainage (ICD) was placed in view of persistent hypoxia, shock and presence of extensive subcutaneous emphysema and the BP picked up to 90/60 mm Hg with saturation of 94%. A CT neck with thorax showed extensive subcutaneous emphysema, pneumo-mediastinum, sub-segmental collapse of the left upper lobe, right sided pneumothorax and a wall irregularity in the trachea 1 cm above carina-suggestive of tracheal rupture [Fig.1]. On reassessing the patient, post-CT scan there was a BP drop to 80/60 mm Hg. As the patient did not improve significantly, an anterior mediastinal ICD was placed by cardio-thoracic vascular surgeon (CTVS) to decompress the heart [Fig.2]. She improved vitally with a HR of 100/min, BP of 120/90 mm Hg and SpO2 improving to 97%.
Owing to the short history she was started on oseltamivir but bronchoscopy and lavage grew methicillin-resistant Staphylococcus aureus (MRSA) and septate fungal elements and was started on antibiotics and anti-fungal injections. Bronchoscopy revealed membranous lesion over the anterior aspect of trachea 1-2 cm above carina. Right main bronchus had blood clots and the left main bronchus showed nodular infiltration. Patient was managed with conservative therapy for the tracheal rent with antibiotics, anti-fungal, mechanical ventilation and inotropic support for 7 days after which she succumbed to severe sepsis. Our final diagnosis was bilateral pneumothorax and pneumomediastinum with obstructive shock, spontaneous TBI secondary to LRTI.
Case 2
A 42-year-old obese female, known case of bronchial asthma on long term steroids presented with breathing difficulty since 1 week, worsened acutely since 3-4 hours with altered sensorium since 1 day. She was previously on inhaled steroids for a period of 10 years. On arrival, airway was threatened with poor respiratory efforts on bag and mask ventilation (BMV) with HR of 120/min, BP of 70 mm systolic and saturation of 70% room air. Patient was started on 100% oxygen via BMV and the saturation improved to 80%. Bedside ABG showed severe respiratory and lactic acidosis with pH 7.021, pCO2 99.7 and pO2 70.7 and HCO3 22.4 with lactate of 16 mmol/L.
Patient was intubated in view of hypercapnia and hypoxia with respiratory and lactic acidosis. Intubation was easy and uneventful. Post-intubation HR was 108/min, BP 90/60 mm Hg and SpO2 88%. On attempting POCUS (point of care ultrasonography) and FOCUS (focussed cardiac ultrasonography) bedside, only hyper-echogenicity was visible with inability to see structures below which raised the suspicion of subcutaneous emphysema. A CT thorax was done which confirmed subcutaneous emphysema (which was missed clinically due to the obesity), posterior tracheal wall irregularity at level of T3 with air column posteriorly suggestive of tracheal injury, and bilateral pneumothorax left more than right with pneumo-mediastinum and ET tube in place [Fig.3,4]. Therapeutically bilateral ICD was placed with improvement in the vitals. Patient was started on antibiotics, inotropic support and mechanical ventilation. However, the patient succumbed to the overwhelming sepsis on day 4 of hospital stay.
To conclude we had a diagnosis of type 2 respiratory failure with bilateral pneumothorax and pneumomediastinum due to spontaneous TBI probably secondary to long term steroid use and bronchial asthma.
Discussion
Acute rupture of the trachea is a rare and life-threatening injury that may be fatal if not treated immediately. Localization of the rupture, nature and extent, mechanism, age and pre-existing risk factors have to be considered in order to define the optimal therapeutic option [
4]. Spontaneous rupture of the trachea is an unusual condition. It occurs after sudden increase of air pressure in a weakened upper airway [3]. Mediastinal and subcutaneous emphysema of sudden onset after an effort of retching or coughing is suggestive for a spontaneous tear in the membranous part of the trachea. The patient usually presents with dyspnea, cyanosis and severe respiratory distress [
5]. Common causes of spontaneous TBI are congenital tracheal diverticulum, tracheal bronchus, airway or mediastinal neoplasms, tracheal inflammation, use of inhaled corticosteroids [2-4]. Other important risk factors are age, poor medical history, short stature, chronic obstructive pulmonary disease, tracheomalacia [
5].
Diagnosis of tracheal rupture is mainly based on clinical signs (sudden onset of the pneumomediastinum and subcutaneous emphysema of the upper thorax diffusing to the neck). It can be confirmed on X-ray chest. Pneumothorax occurs if the tracheal air leak communicates with the pleural space due to a tear of the mediastinal pleura [
6]. Computerised tomography with the appropriated window settings allows direct visualization of the tracheal injury in most of the cases [
7]. Bronchoscopy is the gold standard tool for measuring the size and extent of trachea-bronchial tree injuries. However, small tears can be missed on bronchoscopy too [
7]. After one-look laryngoscopy, a single attempt to gently pass the endotracheal tube is made under direct vision. Standby FONA (front of neck access) team and bronchoscopy are safe strategies if intubation is not feasible [
7,
8]. Surgery is the preferred treatment for patients with acute tracheal rupture [
8]. However, conservative management is an alternative for patients unsuitable for surgery and small tears, with a reasonable chance of spontaneous sealing and uneventful recovery [
8,
9-
11]. According to the majority of authors, early surgical repair in healthy tissues remain the therapy of choice [
1,
2,
7,
10,
12,
13]. According to Massard [
14], when deciding for conservative treatment and in case of its failure, one should be aware that a later operation is not a valuable alternative: the chances of success of a delayed repair are jeopardized by the patient’s poor general condition and by local infection or inflammation. The proposed medical treatment consists of humidified air, broad-spectrum antibiotics and chest physiotherapy. Though different approaches are mentioned about treatment modalities it is up to the clinician to choose the most feasible option with securing of airway taking preference over others.
Conclusion
We report two cases of trachea-bronchial tree injury, one secondary to an LRTI and the other secondary to bronchial asthma with prolonged steroid use. Both were managed conservatively as the rents were small, but both patients did not survive. Spontaneous TBI are life-threatening, under reported, rare and difficult to diagnose and has a high mortality rate.
Contributors: JJ: manuscript writing, patient management; SM: manuscript editing, patient management; HM: critical inputs into the manuscript. AL will act as a study guarantor. All authors approved the final version of this manuscript and are responsible for all aspects of this study.
Funding: None; Competing interests: None stated.
References
- Massard G, Rouge C, Dabbagh A, Kessler R, Hentz JG, Roeslin N, et al. Tracheobronchial lacerations after intubation and tracheostomy. Ann Thorac Surg. 1996;61:1483-1487.
- Marty-Ane CH, Picard E, Jonquet O, Mary H. Membranous tracheal rupture after endotracheal intubation. Ann of Thor Surg. 1995;60:1367-1371.
- Regragui IA, Fagan AM, Natrajan KM. Tracheal rupture after tracheal intubation. Br J Anaesthesia. 1994;72:705-706.
- Zettl R, Waydhas C, Biberthaler P, Lewan U, Riedl V, Duswald KH, et al. Nonsurgical treatment of a severe tracheal rupture after endotracheal intubation. Crit Care Med. 1999;27:661-663.
- Chen EH, Logman ZM, Glass PS, Bilfinger TV. A case of tracheal injury after emergent endotracheal intubation: a review of the literature and causalities. Anesthesia & Analgesia. 2001;93:1270-1271.
- Chen JD, Shanmuganathan K, Mirvis SE, Killeen KL, Dutton RP. Using CT to diagnose tracheal rupture. Am J Roentgenol. 2002;178:241.
- Kaloud H, Smolle-Juettner FM, Prause G, List WF. Iatrogenic ruptures of the tracheobronchial tree. Chest. 1997;112:774-778.
- Borasio P, Ardissone F, Chiampo G. Post-intubation tracheal rupture. A report on ten cases. Eur J Cardio-Thor Surg. 1997;12:98-100.
- Nakamori Y, Hayakata T, Fujimi S, Satou K, Tanaka C, Ogura H, et al. Tracheal rupture diagnosed with virtual bronchoscopy and managed nonoperatively: a case report. J Trauma-Injury Infection & Crit Care. 2002;53:369-371.
- Van Klarenbosch J, Meyer J, De Lange JJ. Tracheal rupture after tracheal intubation. Br J Anaesthesia. 1994;73:550-551.
- Angelillo-Mackinlay T. Transcervical repair of distal membranous tracheal laceration. Ann Thorac Surg. 1995;59:531-532.
- Hofmann HS, Rettig G, Radke J, Neef H, Silber RE. Iatrogenic ruptures of the tracheobronchial tree. Eur J Cardio Thor Surg. 2002;21:649-652.
- Van Klarenbosch J, Meyer J, De Lange JJ. Tracheal rupture after tracheal intubation. Br J Anaesthesia. 1994;73:550-551.
- Massard G, Hentz JG, Wihlm JM. Reply to the comment: Tracheobronchial laceration after double-lumen intubation for thoracic procedures. Ann Thorac Surg. 1998;65:1838-1839.