6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ffa48d36000000330a000001000100
6go6ckt5b5idvals|3106
6go6ckt5b5|2000F757Tab_Articles|Fulltext
Introduction
Bile duct injury in any variety of cholecystectomy is a known complication. Most of the time it arises out of misinterpretation of anatomy rather than a genuine variant of anatomy. Higher the injury at the level of hilum most difficult it is to treat. In literature search, we could not encounter any case with complete hilar injury extending up to second order biliary ducts and the whole biliary hilum was resected along with gall bladder specimen.
Case Report
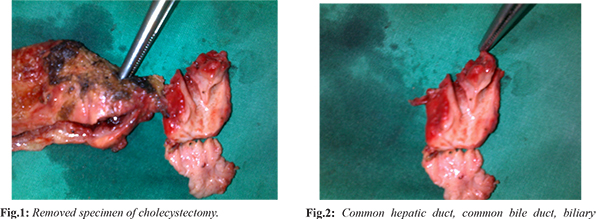
A middle-aged male patient presented with acute cholecystitis, he was investigated and posted for laparoscopic cholecystectomy by a surgeon. During surgery, the surgeon encountered bile duct injury. He noticed the free flow of bile from the hilar area of the liver. He converted to open with right paramedian incision and intra-operatively telephone call was received. Upon examination, it was revealed that bile was coming from multiple areas within the hilum. The bile duct was not visible and along with that right hepatic artery was also not visible but the entire length of the portal vein was visible. Multiple clips were found on the lower end of CBD (common bile duct) and one clip on the right hepatic artery. The proximal end of CHD (common hepatic duct) was not appreciated hence decision to dissect the specimen was made. In the specimen, we found gall bladder, CBD, the entire length of CHD, the confluence of the right and left duct up 2.5 cm on either side [Fig.1,2].
This injury of the bile duct cannot be classified with any of the available, existing classification systems. The injury was extending upto second order biliary ducts within the liver. We managed the patient with the multiple infant feeding tubes inserted in every sectoral duct: right anterior sectoral, right posterior sectoral, segment 4 duct, segment 2 duct and segment 3 duct; and multiple drains in Morrison’s pouch [Fig.3]. The right hepatic artery was repaired with 8.0 prolene interrupted sutures. Post-operatively patient recovered with a controlled biliary fistula. After 2.5 months, MRI with MRCP was done [Fig.4]. A wide hepaticojejunostomy (right and left separate) was done after 2.5 months of index surgery [Fig.5]. At 8 years follow up patient is doing well without any further issues.
Discussion
Bile duct injuries along with hepatic artery injury should be managed in two stages [
2]. Cannulation of sectoral ducts at the time of injury makes the second surgery a little easier especially of this variety. Bile duct injury when recognized intra-operatively carries a better outcome [
3]. Misinterpretation of anatomy is more common than an anomaly in a biliary tree for bile duct injury [
4]. Whenever, such a higher Strasberg injury is encountered, either an expert should be called or if the facility of such is not available then the patient should be either referred to a higher centre after placement of good wide bore, maybe multiple drains [
5]. The patients with type E injuries are more difficult to manage as there is total loss of continuity, it takes long time to localize the fistula along with that it is associated with significant nutritional compromise, electrolyte imbalance, and long-term morbidity to carry the drains. The feeding jejunostomy for such patients is key factor for prevention of post-operative morbidity, especially in presence of complete biliary fistula [
6]. Feeding tube avoids nutritional imbalances and enhances faster recovery of the patient. It maintains gut biliary flora barrier and hence digestion and absorption of fatty foods and fat soluble vitamins. Stenting prevents excessive peri bile duct inflammation, hence the stricture as well as its progression. It also makes the reconstruction during second surgery easier. Surgical treatment should be performed only when the patient is stabilized, and the BDI has been properly classified because the success of the operating procedure depends on the proper and accurate identification of the BDI [
6].
Conclusion
Intraoperatively detected complex bile duct injury carries a better outcome in comparison to post-operatively detected bile duct injury. Creation of controlled biliary fistula in emergency situation is a key to success in management of complex bile duct injury.
Contributors: KB: manuscript writing and editing, patient management. KB will act as a study guarantor. The author approved the final version of this manuscript and is responsible for all aspects of this study.
Funding: None; Competing interests: None stated.
References
- Mercado MA, Domínguez I. Classification and management of bile duct injuries. World J Gastrointest Surg. 2011;3(4):43-48.
- Winslow ER, Fialkowski EA, Linehan DC, Hawkins WG, Picus DD, Strasberg SM. "Sideways": results of repair of biliary injuries using a policy of side-to-side hepatico-jejunostomy. Ann Surg. 2009;249(3):426-434.
- Mercado MA, Chan C, Orozco H, Tielve M, Hinojosa CA. Acute bile duct injury. The need for a high repair. Surg Endosc. 2003;17(9):1351-1355.
- Al-Kubati WR. Bile duct injuries following laparoscopic cholecystectomy: A clinical study. Saudi J Gastroenterol. 2010;16(2):100-104.
- Bansal VK, Misra, MC, Agarwal, AK, Agrawal JB, Agarwal PN, et al. SELSI consensus statement for safe cholecystectomy-Prevention and management of bile duct injury-Part B. Indian J Surg. 2019;10.1007/s12262-019-01994-1.
- Bhatt K, Desai P, Mangukiya D, Kachhadiya D. Bile duct injury: Surgical use of endobiliary stents for the management in emergency situations. Indian J Surg. 2021;83:1146-1152.