6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ffe4ac360000006106000001000a00
6go6ckt5b5idvals|3107
6go6ckt5b5|2000F757Tab_Articles|Fulltext
Introduction
Various risk factors for hepatic abscess formation are alcoholism, diabetes, immuno-compromised states, recent intestinal surgery [
1]. Hepatic abscesses can rupture and spread the infection to the thoracic cavity resulting in the formation of the hepatobronchial fistula rarely [
2]. We report one such case in concomitantly SARS CoV-2 positive patient.
Case Report
A 22 years old male presented to the emergency department of our hospital with chief complaints of fever from past 10 days. Fever was sudden in onset, intermittent, non-documented with chills and rigors and no relieving or aggravating factors. Meanwhile patient also developed gradual onset, progressive right upper abdominal pain radiating to back and aggravated on taking food. The patient also complained of episodes of non-projectile vomiting from the past few days. No history of weight loss or night sweats was present. The patient is a chronic alcoholic and smoker.
In view of fever and the ongoing pandemic of covid-19, the patient was tested for positive SARS-CoV-2 via nasopharyngeal swab. On physical examination, the patient was toxic, febrile having tachycardia and tachypnea. and right hypochondrium tenderness. All blood investigations including liver and renal function tests were normal. Ultrasound abdomen was suggestive of an ill-defined heteroechoic lesion in the right lobe of the liver of approximately 1.5×1 cm with no free fluid in peritoneum. A preliminary diagnosis of liver abscess with covid-19 (positive status) was made.
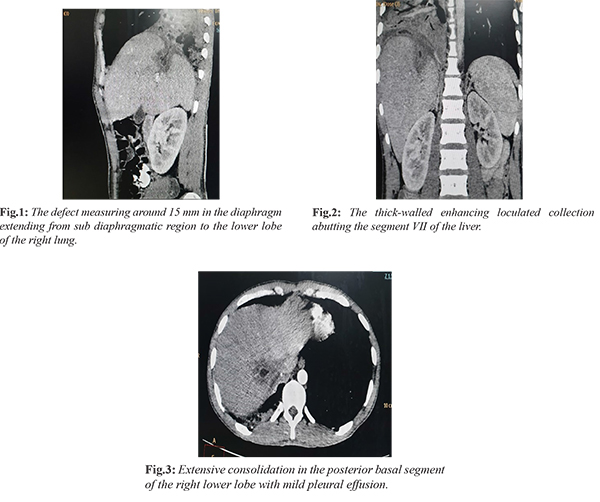
During the course of hospitalization, the patient developed right-sided pleuritic chest pain with productive foul-smelling green colored, copious, mucoid sputum occasionally blood-stained. Sputum was sent for the culture sensitivity which revealed no significant bacterial growth. Suspecting pleuro-pulmonary complication of hepatic abscess, computed tomography imaging of chest with abdomen was done. CT scan was suggestive of extensive consolidation in the posterior basal segment of the right lower lobe with mild pleural effusion which was extending to the sub-diaphragmatic region through the defect measuring 15 mm in the diaphragm and forming the thick-walled enhancing loculated collection abutting the segment VII of the liver [Fig.1-3].
The final diagnosis of hepatobronchial fistula with ruptured liver abscess with covid-19 was made. Percutaneous drainage of the abscess was done under ultrasound guidance and the patient was put-on broad-spectrum antibiotics with coverage for anaerobes with covid-19 treatment as per latest protocols of MoHFW. The patient improved significantly, cough resolved, and was afebrile throughout the hospitalization. Repeat sampling for SARS-COV2 was done as per protocol of ICMR and the third sample was negative. The patient was discharged on day 10 with stable vitals, no signs of desaturation, and symptomatically better condition and accepting orally. The patient was continued on antibiotics regime for 4 weeks and followed up with serial CT scans to ensure resolution of abscess and fistula.
Discussion
Hepatobronchial fistulas are rare entities. They are defined as abnormal communication of a sector of liver parenchyma with a sector of the bronchial tree through a diaphragmatic pathway. Common causes of such fistula include pyogenic liver abscess, amoebic liver abscess, hydatid cyst, and other inflammatory conditions like biliary tree obstruction. Its frequency has mainly reduced due to the use of antibiotics in liver abscess and surgical management of hepatic and pulmonary hydatid cyst [
3]. Hepatobronchial fistulas can be congenital but are chiefly acquired (around 80%) [
4]. Mechanisms for the thoracic spread of the hepatic abscess include direct rupture, lymphatic spread, hematogenous spread and inhalation of E. histolytica cysts [
5]. The death rates can be up to 15% in endemic areas [
6].
Previously the cornerstone of the therapy for heptobronchial fistula has been surgical drainage and correction of the fistulous tract [
7]. But in current times success has been reported with CT and USG guided catheter drainage along with intravenous antibiotics [
8]. The gold standard investigation includes a sinogram or a bronchogram [
9]. MRCP not only helps in confirming the diagnosis but also gives information about the biliary tree and helps with surgical planning [
10].
Conclusion
This is a rare complication of hepatic abscess. The complaint of purulent sputum in a case of liver abscess should raise the suspicion of hepatobronchial fistula.
Contributors: VK: manuscript writing, patient management; AM: manuscript editing, patient management; AC: critical inputs into the manuscript. AC will act as a study guarantor. All authors approved the final version of this manuscript and are responsible for all aspects of this study.
Funding: None; Competing interests: None stated.
References
- Hernandez JL, Ramos C. Pyogenic hepatic abscess: clues for diagnosis in the emergency room. Clin Microbiol Infect. 2001;7:567-570.
- Ala A, Safar-Aly H, Millar A. Metallic cough, and pyogenic abscess. Gastroenterology & Hepatology. 2001;13:967-969.
- Peacock TB. Case in which hydatids were expectorated and one of suppuration of hydatid cyst of the liver communicating with the lungs. Edinburgh Med J. 1850;74:33-46.
- Eryigit H, Oztas S, Urek S, Olgac G, Kurutepe M, Kutlu CA. Management of acquired bronchobiliary fistula: 3 case reports and a literature review. J Cardiothorac Surg. 2007; 2:52.
- Shamsuzzaman SM, Hashiguchi Y. Thoracic amoebiasis. Clin Chest Med. 2002;23:479-492.
- Mbaye PS, Koffi N, Camara P, Burgel PR, Hovette P, Klotz F. Pleuropulmonary manifestations of amebiasis. Rev Pneumol Clin. 1998;54:346-352.
- Stables GI, Irving HC, Simmons AV, Walker BE. Hepatobronchial fistulae complicating amoebiasis, treated by percutaneous catheter drainage. Clin Radiol. 1991;44:354-356.
- Nesper M, McGahan JP. Hepatobronchial fistula with percutaneous pyogenic abscess drainage of the liver. Gastrointest Radiol. 1985;10:129-131.
- Yacoubian HD. Thoracic problems associated with hydatid cysts of the dome of the liver. Surgery. 1976;79:544-548.
- Borrie J, Shaw JHF. Hepatobronchial fistula caused by hydatid disease. Thorax. 1981;36:25-28.