6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ff64eb36000000400a000001000100
6go6ckt5b5idvals|3110
6go6ckt5b5|2000F757Tab_Articles|Fulltext
Introduction
Early in twentieth century, early investigators reported catatonia in 20-50% of the schizophrenic patients [
1,
2]. In the earliest literature of its kind, authors [
3,
4] reported a widespread clinical notion of incidence of catatonic schizophrenia being lesser than the past. In the Diagnostic and Statistical Manual- III (DSM-III), published in 1980 of the American Psychiatric Association, it was stated that, although this type was very common several decades ago, it was found to be then uncommon in Europe and North America. Recent literature on catatonia [
5] suggests the presence of catatonia in 4-15% of schizophrenia patients. In DSM-5, published 2013, diagnostic category of catatonic schizophrenic no longer existed owing to other etiologies causing catatonia. Instead, diagnosis like catatonia due to other mental conditions and that due to medical conditions were introduced. Due to dilemma in diagnosis and under-diagnosis of schizophrenic catatonia, our existing knowledge of its prevalence mainly rests on case reports. Catatonia is seen as medical and psychiatric emergency and hence cases of chronic catatonia are increasingly perceived to be rare. In recent times, recurrent and chronic catatonia cases have been reported by a few, including Grover and Aggarwal M [
6] in 2011, Manjunath et al. [
7] in 2007 and Mukai et al. [
8] in 2011. Varuni A de silva et al. [
9], 2013 reported a medically complicated case of psychotic catatonia of 6 months duration. We hereby report a very rare case of chronic schizophrenic catatonia with a duration of 3 years.
Case Report
Ms A, a 30-year-old unmarried female, 9th grade educated, was brought by relatives to a tertiary care hospital at Mumbai with complaints for 3 years of being immovable, not talking, lying on the bed, passing urine and stools in clothes, not eating by mouth and on Ryles tube (RT) feeds for last 3 years. Patient was admitted in psychiatry ward and detailed history taking and evaluation was made.
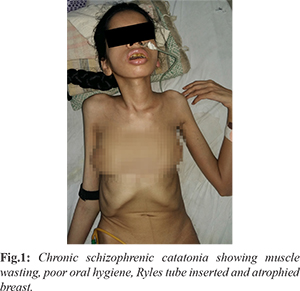
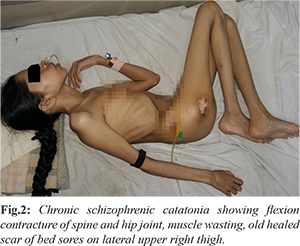
Longitudinally, as reported by her parents,16 years back, without any apparent stressor the patient started complaining of seeing a scary woman in red saree who was not seen by others and becoming fearful that she was trying to harm her. She had behavioral disturbances in form of irritability and agitation. She had multiple episodes of wandering away from home. She also had remarkable socio-occupational impairment (dropout from school). There was no antecedent medical or surgical event. Later in the course of illness patient started having withdrawn behavior, decreased food intake and decreased ambulation for which family members decided to seek medical care. Patient was taken to religious healers many times before but showed no improvement. Patient’s relatives took her to a psychiatrist 3 years back but never continued the treatment beyond 2 weeks, as they did not find improvement as per their expectations. She would develop fever and other minor illness over the period of time for which she would be treated by the local practitioners. Three years back they inserted Ryles tube for feeding to maintain her oral intake at home and relatives would get it changed every 3-4 weekly. Since last 3 years patient had not spoken anything, had developed complete mutism and had not eaten food by mouth by herself. Relatives had to maintain her on RT. Patient was emaciated, had been lying down on bed for last two and a half years, had wasting of muscles and joint stiffness in all large and small joints of all the limbs and vertebral column. She had developed bed sores in the course of illness and amenorrhea. On physical examination, she was averagely built and had extremely poor nourishment. She had RT in situ and oral hygiene was poor. She was lying down on bed in contracted fetal posture in lateral position [Fig.1,2]. Making her lie supine would leave her head maintained above the bed unsupported. On testing joint mobility, attempts to move joints by examiner were impossible due to contractures. Old healed scar marks of bed sores were present on gluteal region bilaterally. Her pulse was 60/min and blood pressure was 90/60 mmHg. Systemic examination was within normal limits.
All necessary investigations were sought on admission [Table 1]. Chest X-ray and electrocardiogram was within normal limits. On admission, liaisons with various other departments were sought and the relevant investigations were undertaken which included-
(a) Neurology: Ocular KF rings were negative, serum ceruloplasmin levels were within normal limits (0.28OD). MRI brain however showed generalized cerebro-cortical atrophy with frontal predominance.
(b) Orthopedics and physiotherapy: MRI spine showed osteopenia of spine with kyphotic deformity. The contractures were planned to be treated conservatively with exercises.
(c) Dermatology: Herpes labialis was treated accordingly.
(d) Gynecology: Serum levels of FSH, LH, prolactin were advised for amenorrhea which were deferred then due to other priority symptoms.
(e) Diet for malnutrition and required oral supplementation. Proper RT feeds were started.
Patient was started on syrup risperidone 0.25 ml on admission. Plan of electroconvulsive therapy was deferred because of high risk involved in short general anesthesia due to ‘difficult airway’ due to flexion contractures at cervical and thoracic spine. On day 5 of admission, she had an episode of fever with tachycardia and hypotension and drop down of serum potassium from 3.5 mEq/L to 2.8 mEq/L which was managed by medical unit. Syrup risperidone was gradually titrated to 4 ml during her ward stay. After 10 days she developed tremors for which oral trihexyphenidyl (2 mg) was given. Orthopedic and physiotherapy treatment for all contractures continued and she was assisted in physiotherapy exercises.
Patient started showing gradual improvement in her catatonic features after 15-20 days. All abnormal blood reports were gradually normalized. Serum creatinine phosphokinase (CPK) levels gradually decreased during her ward stay to 118 IU/L on day 18. Contractures were partially relieved after physical exercises. After 4 weeks, RT was removed and oral feeds were started. She started ambulating. Occupational therapy was sought for rehabilitation. She was discharged after 50 days with tablet risperidone (4 mg), and trihexyphenidyl (4 mg) with 40-50% improvement in her behavioral symptoms.
Discussion
Catatonia, these days is often seen as a historical diagnosis by most of general physicians and even mental health professionals. In its scarce reporting, the cases that get reported or studied in literature are mostly of acute onset. In acutely ill psychiatric inpatients, estimates of catatonia ranging between 5 and 20% may still be reported [
10]. However, reports of long-standing chronic catatonia are rare to find. Catatonic schizophrenia in particular for a duration as long as 3 years is not reported in the literature in recent times as per the best of our knowledge. In a case reported in 2013 [
11], a 41-year-old Asian woman with schizophrenia with intermittent catatonic symptoms of 12 years’ duration was treated successfully with ECTs, the symptoms however were intermittent. Our case, however, had unremitting catatonic symptoms which led to development of serious medical complications.
Devi S. et al. [
12], 2011 reported case of chronic catatonia with physical complications involving meta-carpophalangeal joints treated by ECT. Our patient, due to immobility for a long duration, had developed extensive contractures of most of the small and large joints. Flexion contracture of vertebral column was to such an extent that she had developed truncal deformity. This posed potential risk for short general anesthesia needed for electroconvulsive therapy (ECT) and hence ECTs could not be offered. As noted by van der Heijden FM et al. [
13], 2005 diagnosis of catatonic schizophrenia dropped from 7.8% in 1980-89 to 1.3% in 1990-2001. They also noted that more patients actually fulfill the criteria for diagnosis of catatonia but they are underdiagnosed. Thus, the discussion that this case unveils is many folds. Firstly, the nosological irregularities of catatonia as a clinical occurrence is leading to its probable under-reporting. The lack of consensus while defining chronicity of catatonia and diagnostic classification based on etiology (affective catatonia, organic catatonia etc) may be leading to faulty reporting. Hence this unattended case of chronic catatonia due to schizophrenia may alert all medical professionals to be vigilant of mental health in general and catatonic schizophrenia in particular.
Conclusion
Chronic catatonic schizophrenia may have a broad range of complications. The case signifies the need of early prompt identification and treatment of catatonic symptoms before such dreaded multisystem complications arise. In spite of acknowledgement of declining incidence of symptoms of catatonia in schizophrenia, a rare intricate case like this with incapacitating multi-systemic complications can raise concerns.
Contributors: NSB: Conceptualization, formal analysis, investigation, writing original draft; SRP: conceptualization, validation, formal analysis, supervision. NSB will act as a study guarantor. Both authors approved the final version of this manuscript and are responsible for all aspects of this study.
Funding: None; Competing interests: None stated.
References
- Bleuler E. In: Dementia Praecox or the Group of Schizophrenias. (Trans. J. Zinkin) Zinkin J, editor. New York, NY: International Universities Press; 1950.
- Kraepelin E. Dementia Praecox and Paraphrenia. Edinburgh: E&S Livingstone, 1919.
- Bleuler M. The Schizophrenic Disorders: Long term Patient and Family Studies. New Haven, Yale University Press, 1978.
- Schimel JL, Salzman L, Chodoff P, Grinker RR, Will OA. Changing styles in psychoses and borderline states. American Journal of Psychiatry. 1973:130;151-162.
- Kleinhaus K, Harlap S, Perrin MC, Manor O, Weiser M, Harkavy-Friedman JM, et al. Catatonic schizophrenia: a cohort prospective study. Schizophr Bull. 2012;38(2):331-337.
- Grover S, Aggarwal M. Long-term maintenance lorazepam for catatonia: a case report. Gen Hosp Psychiatry. 2011;33:82-e1.
- Manjunatha N, Saddichha S, Khess CR. Idiopathic recurrent catatonia needs maintenance lorazepam: case report and review. Aust N Z J Psychiatry. 2007;41:625-627.
- Mukai Y, Two A, Jean-Baptiste M. Chronic catatonia with obsessive compulsive disorder symptoms treated with lorazepam, memantine, aripiprazole, fluvoxamine and neurosurgery. BMJ Case Rep. 2011: bcr022011385.
- de Silva VA, Lakmini WD, Heshan N. Gunawardena HN, Hanwella R. Chronic catatonia treated with electroconvulsive therapy: a case report. Journal of Medical Case Reports. 2013;7:219.
- Fink M, Taylor MA. The catatonia syndrome: forgotten but not gone. Arch Gen Psychiatry. 2009;66(11):1173-1177.
- Cupina D, Patil S, Loo C, Chronic catatonic schizophrenia treated successfully with right unilateral ultra-brief pulse electroconvulsive therapy: case report. J ECT. 2013;29:134-136.
- Devi S, Behere RV, Varambally S, Rao NP, Venkatasubramanian G, Gangadhar BN. Physical deformity as sequela of chronic catatonia and response to electroconvulsive therapy: a case report. J ECT. 2011;27(3):e49-50.
- van der Heijden FM, Tuinier S, Arts NJ, Hoogendoorn ML, Kahn RS, Verhoeven WM. Catatonia: disappeared or under-diagnosed? Psychopathology. 2005;38(1):3-8.