6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ffe429370000005a06000001000e00
6go6ckt5b5idvals|3113
6go6ckt5b5|2000F757Tab_Articles|Fulltext
Introduction
The differential diagnosis for oral cystic lesions in neonate includes ranula, dermoid cyst, epidermoid cyst, teratoma, lymphatic malformation, and foregut duplication cyst [
1]. Epidermoid cysts are benign cystic lesions lined by squamous epithelium. Head and neck constitute 2-7% of all epidermoid cysts, bucco-alveolar lesions account for 1-1.5% of all epidermoid body lesions [
1,
2]. Mostly asymptomatic, these patients present after 20 to 30 years of age [
1]. Our reported case presented at birth with difficulty in feeding. To the best of our knowledge this is the youngest case of sublingual epidermoid cyst reported in English literature till date.
Case Report
A full-term female neonate was born to a 30-year-old gravida 1, para 1 in our institute. Her birth weight was 1.9 kg. Just after birth, the obstetrician noted a swelling on the undersurface of tongue. The baby was unable to breast feed. A pediatric surgery call was made in view of macroglossia. On examination a painless soft cystic lesion of 4.5×3 cm size was present on the undersurface of tongue and displacing the tongue superiorly and to the left. It was non transilluminant, fluctuant to firm in consistency, non-reducible and non-pulsatile. and was distinguishable from normal tongue tissue [Fig.1].

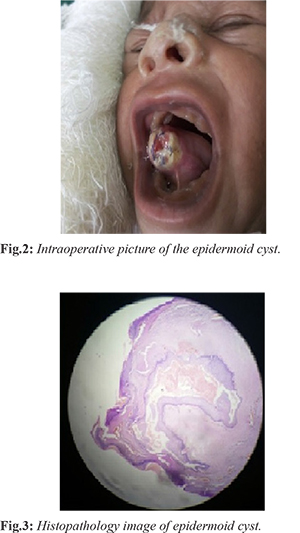
Her laboratory blood count revealed hemoglobin of 15.9 gm% (normal range 12 to 20), total leukocyte count 26000/mm3 (normal range 9000 to 20000) and raised C-reactive protein. High resolution ultrasonography (USG) demonstrated a large swelling mainly over the ventral aspect of tongue with predominantly cystic component suggestive of lymphangioma or ranula. The patient was taken up for surgery on 2nd post-natal day, under sedation and aspiration of cyst contents was done with an 18G needle followed by marsupialization of the cyst. Post marsupialization a 2×1 cm full thickness wall of cyst was excised. Excised cyst wall was sent for histopathological examination [Fig.2]. The patient was then shifted to NICU for post-operative care. The patient was started on oral feed on first post-operative day and discharged next day. Aspirated content was sent for culture and sensitivity which inferred few pus cells. No growth was seen in culture after 48 hrs. Histopathology reported sublingual epidermoid cyst with lining made by epidermis like epithelium and cyst wall had laminated keratin [Fig.3]. The patient was followed up after 3 and 6 months. On follow up the patient was doing well and was taking breast feeds normally.
Discussion
Epidermal inclusion cysts or epidermoid are either congenital or acquired. Congenital cysts are due to defective embryogenesis and are derived from entrapment of ectodermic elements during fusion of first and second brachial arch in intrauterine life [
3]. Acquired cysts occur due to trauma or any surgery in which there is inclusion of epithelium or due to blockage of duct of sebaceous gland. Epidermoid cysts of oral cavity are extremely rare which account for about 0.01% of all cystic lesions of oral cavity [
1,
2]. Epidermoid cysts are differentiated from dermoid cysts as they are lined by epithelium, whereas dermoid is epithelium lined and has skin adnexal structures like hair follicles, sebaceous gland and others. Usually, epidermoid cyst in oral cavity is detected in second and third decade of life, which is mostly asymptomatic.
The swelling in our case was homogenous to normal tongue tissue. But on examination, pediatricians were confused and they diagnosed it as macroglossia for which pediatric surgery reference was made. Repeat clinical examination revealed it as cystic mass which on magnetic resonance imaging (MRI) raised suspicion of an epidermoid cyst or ranula foregut duplication cyst for which excision/ marsupialization was planned.
Conclusion
This case is being reported to re-emphasize the importance of epidermoid cyst as a differential diagnosis of any swelling on under surface of tongue since birth. Referring physicians and pediatricians should keep sublingual epidermoid cyst as differential diagnosis of macroglossia.
Contributors: BKL: manuscript writing, patient management; RMS, SJ: manuscript editing, patient management; SSS, AL, SD, PC: critical inputs into the manuscript. SJ will act as a study guarantor. All authors approved the final version of this manuscript and are responsible for all aspects of this study.
Funding: None; Competing interests: None stated.
References
- Mohta A, Sharma M. Congenital oral cysts in neonates: report of two cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102:e36-38.
- Bitar MA, Kumar S. Plunging congenital epidermoid cyst of the oral cavity. Eur Arch Otorhinolaryngol. 2003;260:223-225.
- Kandogan T, Koç M, Vardar E, Selek E, Sezgin Ö. Sublingual epidermoid cyst: a case report. J Med Case Rep. 2007;1:87.
- Corrêa MS, Fonoff Rde N, Ruschel HC, Parizotto SP, Corrêa FN. Lingual epidermoid cyst: case report in an infant. Pediatr Dent. 2003;25:591-593.
- Oginni F, Oladejo T, Braimah R, Adenekan AT. Sublingual epidermoid cyst in a neonate. Ann Maxillofac Surg. 2014;4:96-98.