6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ffe4a0380000006a07000001000800
6go6ckt5b5idvals|3129
6go6ckt5b5|2000F757Tab_Articles|Fulltext
Introduction
Hydatid cysts, also known as echinococcosis or hydatidosis are swellings caused by infection of parasite
Echinococcus granulosus. Hydatid cyst is commonly seen in the Middle East, South America, North Africa and Australia. Hydatid cysts are mainly seen in two organs, the liver (70%) and lungs (25%) [
1]. Less common sites affected by the disease include the spleen, kidneys, bile ducts, mesentery, heart, brain and the musculoskeletal system. Diagnosis of hydatid cysts are mainly based on cross-sectional imaging techniques such as ultrasound, computed tomography (CT) scans or magnetic resonance imaging (MRI) [
2-
4]. The lesion usually appears as a thin-walled mass with inner membranes and a characteristic cystic look. Aspiration cytology studies of the cyst are also useful in diagnosis but must be done with caution due to the risk of rupture and leakage of the cyst fluid [
5,
6]. Serological investigations like ELISA, latex agglutination and immune electrophoresis also play a role in diagnosis [
7]. Hydatid cysts of the neck are an exceedingly rare presentation of the disease accounting for less than 1% of all reported cases. In this paper a case with an unusual localization of primary hydatid cyst in the right posterior triangle region of the neck is presented and discussed with the aim of showing that hydatid cyst though rare, should be kept in consideration by clinicians while investigating a case of neck swelling.
Case Report
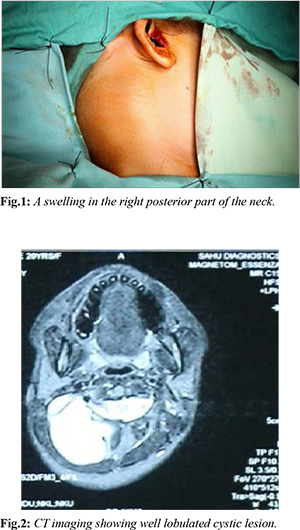
A 26-year-old female presented to the hospital with complaints of swelling in the right posterior part of her neck which first appeared 8 years back [Fig.1]. She visited a local hospital where swelling was diagnosed to be a hydatid cyst. She was placed on a course of albendazole for two years following which the swelling subsided. Patient was subsequently asymptomatic until two years back when the swelling reappeared at the same site. On recurrence the swelling was insidious in onset and painless, initially the size of a pea but gradually progressed in size to approximately 5×5 cm in size. There were no complaints of pain, dysphagia, difficulty in breathing, fever, weight loss, or exposure to Echinococcus such as contact with cats or dogs. Other possible differential diagnosis included dermoid cyst, tubercular lymph node and brachial cyst. On examination she was found to have a swelling in the right posterosuperior part of her neck which was around 5×4 centimeters (cms) in size and extending upwards to around 1 cm behind the pinna. On palpation the swelling was soft, fluctuant and mobile. An ultrasound scan of the swelling was done which revealed a multicystic swelling with a strong possibility of being a hydatid cyst. Subsequently an FNAC of the swelling was done which reported the swelling as being comprised of clear watery fluid with numerous polymorphs and calcified scolices which were indicative of a long standing hydatid cyst. CT imaging of the lesion was done which showed the lesion to be a well lobulated cystic lesion 5.8×4.3×5 cms in size located in the posterior triangle of neck beneath the splenius and within the semispinalis muscle and filled with fluid [Fig.2]. An MRI scan was also done as per advice from neurosurgery to rule out possibility of intracranial involvement and involvement of the vertebral column. MRI report revealed the mass to be a well-defined, thick walled, irregular cystic lesion in the posterior spinal area on the right side of the neck in the intramuscular plane.
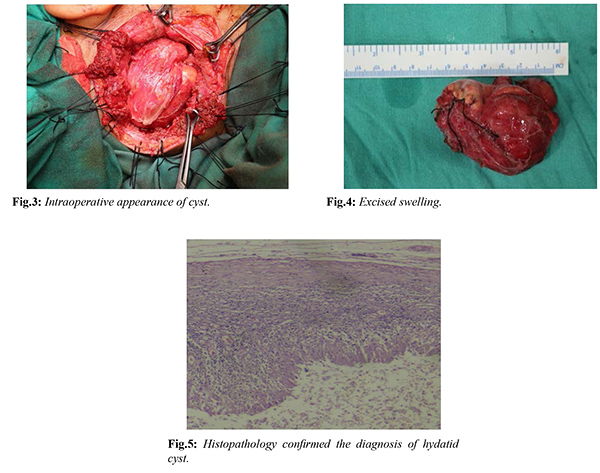
Under albendazole cover patient underwent surgical excision of mass under general anaesthesia. An incision was placed in the neck, subplatysmal flap was elevated and sternocleidomastoid and splenius capitis muscles were divided to expose the swelling. Intraoperatively the cyst was noted to be thick walled mimicking the appearance of a dermoid cyst [Fig.3]. Swelling was dissected away from the surrounding muscles and the prevertebral fascia posteriorly, all margins demarcated and subsequently excised in and sent for histopathological examination (HPE) [Fig.4]. Special precaution was taken during procedure to avoid spillage of the cystic components. Procedure was uneventful. Post-procedure, patient was stable with no nerve deficits and started on antibiotics and albendazole. Patient recovered well and operative site healed without any issue. She was discharged a week after surgery and reviewed with the HPE report of the swelling after 2 weeks which confirmed the swelling as a hydatid cyst [Fig.5]. Albendazole cover was continued for a further 3 months post-operatively with monitoring of her renal parameters to watch out for toxicity. Patient was asymptomatic with no recurrence of the lesion in follow-up period.
Discussion
The parasite
Echinococcus granulosus has a unique life cycle which alternates between herbivores and carnivores. The germinative layer is responsible for producing the scolices that represent the larval stage of
Echinococcus infection [
8]. Diagnosis of hydatid cysts are made by a combination of history taking, clinical examination, imaging studies, serological investigations and aspiration cytology. Ismail Iynen et al. reported a similar case of a hydatid cyst in the supraclavicular region with no involvement of any other organs [
9]. MRI scans show the multiloculated cystic lesion in neck. Fine needle aspiration cytology yields fluid aspirate and smear shows fragment of laminated membrane, which suggests presence of hydatid cyst [
10]. MRI scans of neck can also help in better and adequate surgical panning as surgical excision remains the treatment of choice for hydatid cysts of the head and neck region with the best long term results. Medical treatment is mostly used to sterilize the cyst, reduce the risk of intraoperative contamination and reduce the chance of recurrence. Albendazole is the drug of choice in medical management of hydatid cyst although other imidazole derivatives like mebendazole may be used as well. Albendazole is usually given at a dose of 10 mg/kg/day for 3-6 weeks before surgery to sterilize the cyst [
11]. During surgery special care should be taken not to spill the hydatid fluid. To achieve this, precautions are to be taken which include packing the operative field with povidone iodine soaked sponges, reducing the tension within the cyst by aspirating some of the hydatid fluid, instilling scolicidal agents like hypertonic saline, 5% silver nitrate or formalin in the operative field and use of a suction cone. After the operation, the patient should continue albendazole for at least another 6-8 weeks to kill off any daughter cysts that might have survived the procedure and thereby prevent any chance of recurrence.
Conclusion
Isolated hydatid cyst is an exceptional and rare clinical presentation of neck masses, it should be considered in the presence of any cystic mass of the neck essentially in endemic regions. Ultrasound and MRI scans facilitate diagnostic and therapeutic procedures in order to achieve complete surgical excision which is main line of management, although prevention remains the essential treatment.
Contributors: RM, AN: manuscript writing, patient management; NMN, JRD: manuscript editing, patient management; GG, AM: critical inputs into the manuscript; NH: cyto- and histo-pathology, along with manuscript revision. JRD will act as a study guarantor. All authors approved the final version of this manuscript and are responsible for all aspects of this study.
Funding: None; Competing interests: None stated.
References
- Katilmis H, Ozturckan S, OzdemirI I, Guvenc I.A, Ozturan S. Primary hydatid cyst of the neck. American Journal of Otolaryngology Head and Neck Medicine and Surgery. 2007;28:205-207.
- Akal M, Kara M. Primary hydatid cyst of the posterior cervical triangle. Journal of Laryngology & Otology. 2002;116:153-155.
- Iynen I, Sogut O, Guldur ME, Kose R, Kaya H, Bozkus F. Primary hydatid cyst: an unusual cause of a mass in the supraclavicular region of the neck. Journal of Clinical Medicine Research. 2011;3:52-54.
- Jarboui S, Hlel A, Daghfous A, Bakkey MA, Sboui I. Unusual location of primary hydatid cyst: soft tissue mass in the supraclavicular region of the neck. Hindawi Publishing Corporation - Case Reports in Medicine. 2012;484638:4.
- Nath K, Prabhakar G, Nagar RC. Primary hydatid cyst of neck muscles. Indian Journal of Pediatrics. 2002;69 (11):997- 998.
- Ahmad S, Jalil S, Saleem Y, Suleman BA, Chughtai N. Hydatid cysts at unusual sites: Reports of two cases in the neck and breast. Journal of the Pakistan Medical Association. 2010;60(3):232-234.
- Khalifa R, Nasser F, Elsetouhy A, Farag I. Hydatid cyst of the neck. A case report and literature review. Egyptian Journal of Ear, Nose, Throat and Allied Sciences. 2016;17:103-105.
- Hamad MNM. Echinococcus granulosus, Life Cycle. 2010.13140/RG.2.2.36658.71361. Available at https://www.researchgate.net/publication/323943544_Echinococcus_granulosus_LifeCycle. Accessed on December 5, 2021.
- Singal R, Mittal A, Garg M, Zaman M, Chaudhry M, Singhal S, et al. Unusual location of primary hydatid cyst diagnosed on aspiration cytology. J Cosmet Dermatol. 2017;16:e42-e44.
- Soosaraei M, Alizadeh S, Fakhar M, Banimostafavi ES. The mandibular angle hydatid cyst mimicking branchial cleft cyst: A Case Report. Iran J Parasitol. 2016;11(4):591-594.
- Goyal P, Ghosh S, Sehgal S, Panda I, Kumar A, Singh S, et al. Primary multilocular hydatid cyst of neck with unique presentation: a rare case report and literature review. Head Neck Pathol. 2014;8(3):334-338.