6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ffeca038000000aa06000001000400
6go6ckt5b5idvals|3131
6go6ckt5b5|2000F757Tab_Articles|Fulltext
Background
Laparoscopic sleeve gastrectomy and Roux-en-Y gastric bypass are the two most commonly performed bariatric procedures in Australia [
1]. In recent years, an adjunct restrictive silastic band or silicone ring devices (MiniMizer ring) placed on the gastric pouch has gained much popularity to assist weight loss maintenance through improved restriction and reduction of post-operative dumping syndrome [
2]. This is on the notion that pouch dilatation can be responsible for insufficient weight loss and/or weight regain in the long-term [
3]. In particular, MiniMizer ring is commonly implanted as it requires only very limited dissection at the lesser curvature, adding minimal time to duration of surgery [
4]. Although there is a growing body of evidence that these rings are associated with improved excess weight loss in long-term [
3,
5,
6], it comes at the cost of potential band-related complications such as vomiting, band migration, erosion and bleeding, which are reported up to 7% of the cases [
3,
6,
7]. Therefore, surgeons need to be aware of potential complications from these devices and be able to manage them with appropriate utilisation of endoscope and surgery.
Case Report
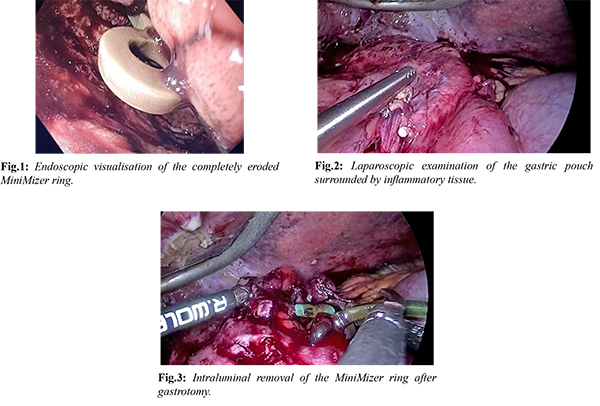
A 43-year-old female presented to our emergency department with two days of abdominal pain and melena, associated with significant hemodynamic instability. Her background includes a previous sleeve gastrectomy which was later converted to a Roux-en-Y bypass for weight regain with placement of a MiniMizer gastric ring 3 years ago. Resuscitation including blood products were given. At urgent endoscopy, her MiniMizer ring was found to have eroded into her gastric lumen, just proximal to her gastro-jejunostomy, causing bleeding with a visible vessel within an ulcer which was treated with adrenaline and gold probe. Despite this, she continued to have ongoing bleeding in our intensive care unit, requiring six units of packed cells transfusion. On this basis, she was taken for laparoscopic removal of her MiniMizer ring.
At laparoscopy, despite extensive adhesiolysis around the liver and gastric pouch, the ring was not visible. There was a lot of inflammatory tissue in the area between the liver, gastro-jejunostomy and remnant stomach. Intra-operative gastroscopy was performed in order to identify the position of the eroded ring intra-luminally and under laparoscopic vision, we could identify the light of the gastroscope. A gastrotomy was then made with sharp diathermy and extended with Ligasure device to involve the gastro-jejunostomy. The buckle of the ring was visible intra-luminally and was cut with scissors and retrieved. After haemostasis was achieved with diathermy the gastrotomy was closed with laparoscopic continuous 3-0 absorbable V-lock sutures. A leak test with gastroscopy confirmed no leak, a patent gastro-jejunostomy and satisfactory haemostasis intra-luminally. The patient was discharged twelve days later on a normal diet and no further transfusion requirement whilst in hospital.
Discussion
Common complications of silastic rings are related to obstruction and migration [
1,
8]. In previous case reports detailing removal of migrated rings, the rings are usually easily visible on laparoscopy with minimal adhesiolysis [1,8]. As far as we are aware there is only one case report published of erosion and bleeding caused by silastic rings. The case described by Franco-Martinez et al. showed erosion of a ring into the bypassed stomach of a patient who had a Fobi-pouch operation, a variation to the Roux-en-Y gastric bypass, requiring resection of the stomach [
9]. In our case we were able to avoid resection and the greater morbidity associated
with it.
Tan et al. [
8] proposed an algorithm detailing determination of migration versus erosion with gastroscopy and endoscopic removal as first line followed by diagnostic laparoscopy and removal if endoscopy was unsuccessful. In our case the band was unable to be safely removed with endoscopy or laparoscopy alone. Endoscopically the buckle was not fully visible. Endoscopic retrieval of bands is ordinarily achieved with JAG wire and cutting the band requires a manual Soehendra lithotripter which was not available with us and we were not familiar with the use of these instruments. We were also wary of laparoscopic removal as we did not want to disrupt any phlegmonous tissue associated with erosion. The significant fibrotic tissue surrounding the remnant stomach and gastrojejunostomy site also made it impossible to identify the position of the ring via laparoscopy alone. With the aid of intra-operative gastroscopy, we were able to identify that the ring was proximal to the gastrojejunostomy site and achieved intraluminal retrieval of the ring via laparoscopy.
Conclusion
We present this case report to highlight this morbid complication of a silastic band 3 years post-operatively and to also present a novel method for intra-luminal removal in a case where endoscopic or laparoscopic retrieval was not possible as independent methods. As evidenced in this case, visualisation of these rings when eroded may not always be possible. Compared to gastric laparoscopic bands, which normally have a port and tubing that can guide approximate location of the band, silastic rings are small and can be difficult to be visualised in the setting of partial or complete erosion with inflammatory tissue around the gastric pouch. This approach provides insight into safe laparoscopic removal of completely eroded silastic rings where inflammatory tissue obscures visualisation of relevant anatomy.
Contributors: EYL: manuscript writing, patient management; SSP: manuscript editing, patient management; EW: critical inputs into the manuscript. EL will act as a study guarantor. All authors approved the final version of this manuscript and are responsible for all aspects of this study.
Funding: None; Competing interests: None stated.
References
- Huang YC, Mitchell D. Multiple concurrent complications of Roux-en-Y gastric bypass with MiniMizer gastric ring-alimentary limb intussusception through slipped ring into pouch, with remnant stomach internal herniation. J Surg Case Rep. 2020;2020(3):rjaa033.
- Rasera I, Jr, Coelho TH, Ravelli MN, Oliveira MR, Leite CV, Naresse LE, et al. A comparative, prospective and randomized evaluation of Roux-en-Y gastric bypass with and without the silastic ring: A 2-year follow up preliminary report on weight loss and quality of life. Obes Surg. 2016;26(4):762-768.
- Lemmens L. Banded gastric bypass: better long-term results? A cohort study with minimum 5-year follow-up. Obes Surg. 2017;27(4):864-872.
- Karcz WK, Karcz-Socha I, Marjanovic G, Kuesters S, Goos M, Hopt UT, et al. To band or not to band--early results of banded sleeve gastrectomy. Obes Surg. 2014;24(4):660-665.
- Awad W, Garay A, Martinez C. Ten years experience of banded gastric bypass: does it make a difference? Obes Surg. 2012;22(2):271-278.
- Bessler M, Daud A, Kim T, DiGiorgi M. Prospective randomized trial of banded versus nonbanded gastric bypass for the super obese: early results. Surg Obes Relat Dis. 2007;3(4):480-484; discussion 4-5.
- Moon RC, Frommelt A, Teixeira AF, Jawad MA. Comparison of banded versus non-banded Roux-en-Y gastric bypass: a series of 1150 patients at a single institution. Obes Surg. 2018;28(1):212-217.
- Tan EW, Luck T, Huo A, Cheng Y. First case of the migrating MiniMizer ring. ANZ J Surg. 2019;89(7-8):972-974.
- Franco-Martinez AM, Guraieb-Trueba M, Castaneda-Sepulveda R, Flores-Villalba EA, Rojas-Mendez J. Silastic band erosion in the bypassed stomach after Fobi-pouch. Int J Surg Case Rep. 2018;47:22-24.