6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ff64df38000000660a000001000100
Introduction
The ductal eccrine carcinoma (DEC) is a rare skin neoplasm that originates from the eccrine sweat glands, representing around 0.01% of all cutaneous neoplasia [1]. Sweat gland tumors can be subdivided into four groups: eccrine, apocrine, mixed origin, and unclassifiable besides being classified into malignant and benign. The benign entities include hidradenoma, syringoma, poroma, and others. The eccrine malignant tumors are porocarcinoma, malignant cylindroma, mucinous carcinoma, adenoid cystic carcinoma, among others. The DEC is among the unclassified entities [2]. Due to its morphology and infiltrative pattern in the dermis extending to the subcutaneous tissue and the low incidence it can be misdiagnosed as invasive breast carcinoma. Due to the rarity of this entity, there are no current guidelines for the diagnosis and treatment; there aren't also well-defined risk factors.
Case Report
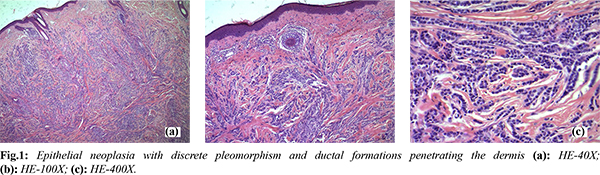
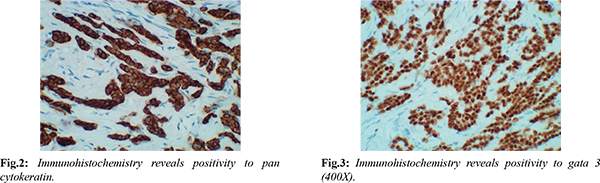
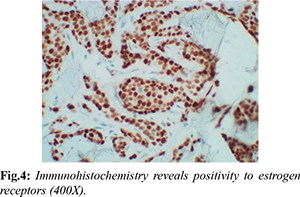
We present a case of a 62-year-old woman with a nodular ulcerated lesion in the frontal region of the scalp that had been persistent for about a year. Due to visibility of lesion for last two months, the patient sought medical help. Incisional biopsy revealed cutaneous adnexal tumor; excision of the lesion was recommended for further clarity. The histopathological findings of the excised lesion showed epithelial neoplasia with discrete pleomorphism and ductal formations penetrating the dermis [Fig.1]. The immunohistochemistry showed positive to pan-cytokeratin AE1/AE3 [Fig.2], gata-3 [Fig.3], and strongly positive for estrogen receptors (100% of the neoplastic cells) [Fig.4]. It was negative for mammaglobin, GCDFP-15, progesterone receptor, and HER2. After excluding the possibility of a cutaneous metastases of breast carcinoma (CMBC) through clinical evaluation and complementary exams, it was then suggested that it could be a DEC. After 14 months of follow-up, she remains disease-free and in good health.
Discussion
The difficulty in the diagnosis not only relies on the rarity of the entity but in many cases the biopsy has insufficient depth to analyze the ductal proliferation in the hypodermis. Besides this there is a resemblance with invasive breast carcinoma; approximately 25% of patients with breast carcinoma can have cutaneous metastasis. The main difference is in number; DEC is usually an only lesion as presented in this case report whereas CMBC are multiple cutaneous lesions [3,4].
The immunohistochemistry is positive for most simple cytokeratins (CK7, 8, 18, and 19). It also has estrogen and progesterone receptors and CEA, c-erbB-2, S100, GCDFP-15 in variable degrees. The mammaglobin is positive in metastatic breast cancer and negative in the DEC. Markers as HER2 have little diagnostic value since both entities can express these antibodies. Due to the resemblance and different clinical courses between the DEC and CMBC an immunohistochemistry panel has been proposed along with an extended investigation [4,5].
Conclusion
The case of the 62-year-old woman with a persistent nodular ulcerated lesion on the scalp highlights the importance of prompt diagnosis and treatment of cutaneous adnexal tumors. The histopathology findings suggest that the tumor could be a rare type of cutaneous adnexal tumor called a DEC. Positive immunohistochemistry for pan-cytokeratin AE1/AE3, gata-3, and estrogen receptors supports the diagnosis. The excision of the tumor resulted in a disease-free status for the patient after 14 months of follow-up. Long-term monitoring may be necessary to ensure that the tumor does not recur or metastasize.
Contributors: JCMK drafted the work with the help of CK and DCO and YWPS revised it. CK will act as a study guarantor. All authors approved the final version of this manuscript and are responsible for all aspects of this study.
Funding: None; Competing interests: None stated.
References
- Sidiropoulos M, Sade S, Al-Habeeb A, Ghazarian D. Syringoid eccrine carcinoma: a clinicopathological and immunohistochemical study of four cases. J Clin Pathol. 2011;64(9):788-792.
- Kaseb H, Babiker HM. Cancer, An Overview of Eccrine Carcinoma. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan. 2022 Jul 10.
- Swanson PE, Cherwitz DL, Neumann MP, Wick MR. Eccrine sweat gland carcinoma: an histologic and immunohistochemical study of 32 cases. J Cutan Pathol. 1987;14(2):65-86.
- Ohnishi T, Kaneko S, Egi M, Takizawa H, Watanabe S. Syringoid eccrine carcinoma: report of a case with immunohistochemical analysis of cytokeratin expression. Am J Dermatopathol. 2002;24(5):409-413.
- Rollins-Raval M, Chivukula M, Tseng GC, Jukic D, Dabbs DJ. An immunohistochemical panel to differentiate metastatic breast carcinoma to skin from primary sweat gland carcinomas with a review of the literature. Arch Pathol Lab Med. 2011;135(8):975-983.