6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ffa8fe380000007106000001001800
Introduction
The prevalence range of placental cysts is between 2% and 7% [1]. In term pregnancies, the incidence of placental cysts is 7% [2]. Generally, these cysts go unnoticed, but if they are large and located near the umbilical cord, they can compromise blood flow and cause fetal growth retardation [3]. In this case report, we present the case of a pregnant woman who presented to our hospital at term with a subchorionic placental cyst and fetal growth restriction.
Case Report
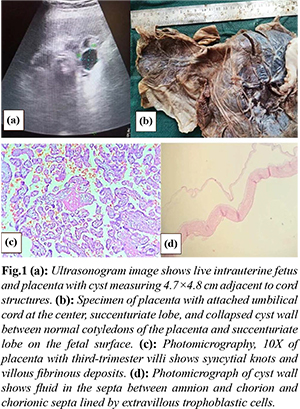
This 26-year-old primigravida presented to the Obstetrics outpatient department at 40 weeks of gestation with a history of pain abdomen for 10 days. On abdominal examination, the uterus was at term with a cephalic presentation, relaxed, and the fetal heart rate was 130/minute. Per speculum examination revealed candidiasis, while per vaginal examination showed that the cervix was soft, and the pelvis was adequate. Ultrasonogram revealed a well-defined smooth marginated thin-walled cystic lesion noted in the lower pole of the placenta of size 4.7×4.8 cm extending from the fetal to the maternal surface adjacent to the cord and succenturiate lobe. No evidence of septations or solid intramural components was observed. There was no apparent color uptake (blood flow signal). The rest of the placenta visualized was normal. The amniotic fluid index was 4, suggestive of oligohydramnios. The patient was shifted to the emergency operation theatre (OT), and lower section caesarean section (LSCS) was performed with the delivery of a single live male baby with a birth weight of 2.4 kg. Apgar score was 8 and 9 at 1 and 5 minutes, respectively. The baby cried immediately after birth. The liquor was dark-colored, and meconium stained. Macroscopically, a collapsed cyst wall between the fetal surface and succenturiate lobe was observed. Microscopic examination revealed fluid-filled spaces beneath the chorionic plate. Extra villous trophoblast cells (X cells) were found in the cyst wall.
Discussion
Placental morphology variation is associated with fetal and maternal conditions like hydrops, polycystic ovarian disease, hypertension, and diabetes [4]. Placental cysts often occur in maternal diabetes and Rh incompatibility. A large placental cyst on the fetal side can cause fetal growth restriction, infarction, hematoma, and neonatal morbidity [4]. If the cyst appears at the placental cord insertion site, fetal growth restriction occurs due to compromised blood supply [5].
The pathogenesis of cysts is reported to have a relationship with low circulation, hypoxia, and fluid secretion by X-cells within the cyst wall. In response to hypoxia, X cells will have an increased capacity of margination and increased vascularity, leading to placental cyst formation [5]. These X cells are seen in the septa, basal plate, and lining of both septal and subchorionic cyst. These X cells have secretory activity, and this can contribute to cyst formation [3]. A pregnancy-associated major basic protein produced by X cells is the major constituent protein in the cyst fluid. These proteins are highly toxic and lead to tissue degeneration and cyst formation [3]. The placental cyst wall is lined by X cell, which is an extra-villous trophoblast that will secrete cyst fluid with prothrombotic properties and finally end up with hemorrhagic events [2]. Microscopically cyst wall is composed of amniotic and chorionic membranes [3]. X cells will be found in the cyst wall. These X cells are clear cubic cells, and the remaining placenta shows increased capillaries, syncytial knots, and indented terminal villi with focal areas of avascular necrosis [2]. Subchorionic cyst are associated with pre-villous deposition of fibrin [6]. The majority of the placental cyst are simple cysts having internal echogenicity similar to amniotic fluid [1]. Analysis of cyst fluid revealed an increase in creatinine, collagen, CRP, tissue factors, Von Willebrand factor, chemokine CXCL4; reduced surfactant D, PS-positive microparticles, a-fetoprotein, ß-HCG, fibrinogen, a2-macroglobulin, and haptoglobin [2].
Differential diagnoses of the placental cyst are sub-amniotic and subchorionic cyst, chorioangioma, cord cyst, and placental lakes [6]. Subchorionic cysts occur as echo-free cavities under the fetal plate, and they do not have blood flow and hence will not give a Doppler signal. It should be differentiated from both subchorionic fibrin deposition and choriangiomas [3]. Subchorionic cysts are diagnosed at first trimester transvaginal ultrasound. Often on serial scans, it remains unchanged, but the size may be increase as the pregnancy progresses [3]. Patients with placental cysts are recommended for regular ultrasonograms to check any increase in size, modification in content that can cause a change in echogenicity, and evidence of hemorrhage. In addition to fetal growth movement, heart rate should also be monitored. To assess the blood flow of the umbilical cord, color doppler is performed [2].
Conclusion
The choice of delivery method should be determined based on the assessment of the risk of placental cyst rupture and fetal growth restriction. An atypical trajectory of the cyst may elevate the risks of traction, compression, and thrombosis. However, in most cases, patients with a placental cyst can undergo a normal delivery.
Contributors: SV: drafting and literature search; PS: conception and editing; PPB: Images and editing. SV will act as a study guarantor. All authors approved the final version of this manuscript and are responsible for all aspects of this study.
Funding: None; Competing interests: None stated.
References
- Elsayes KM, Trout AT, Friedkin AM. Imaging of the placenta: A multimodality pictorial review. RadioGraphics. 2009;29(5):1371-1391.
- Bonasoni MP, Comitini G, Blasi I, Cavazza A, Aguzzoli L. Large subchorionic cyst located at umbilical cord insertion with vascular displacing and intracystic hemorrhage/hematoma: A case report. Fetal Pediatr Pathol. 2022;41(3):468-474.
- Raga F, Ballester MJ, Osborne NG, Bonilla-Musoles F. Subchorionic placental cyst: a cause of fetal growth retardation ultrasound and color-flow Doppler diagnosis and follow-up. J Natl Med Assoc. 1996;88(5):285-288.
- Murlewska J, Respondek-Liberska M, Lusinska A, Poszwa P, Sajdak S. Placental cyst – case study. Prenat Cardiol. 2019;9:51-55.
- Soyama H, Miyamoto M, Sasa H, Yoshida M, Takano M, Furuya K, et al. Multiple placental surface cysts with intracystic hemorrhaging: A case report and review of the literature: Placental surface cysts with hemorrhage. J Obstet Gynaecol Res. 2017;43(8):1346-1349.
- Witters I, Sieprath P, Van Holsbeke C, Theyskens C, Deraedt K. Prenatal diagnosis of multiple large subchorionic placental cysts with intracystic hemorrhage. Facts Views Vis ObGyn. 2017;9(4):223-225.