|
Suneeta Padhy, Shimal Thasneem, Milza Abdul Muhsin, Sanju Sharma Poudel Department of Pathology, Indira Gandhi Memorial Hospital, Male, Maldives.
Corresponding Author:
Dr. Suneeta Padhy Email: suneetapadhy96@gmail.com
Abstract
Background: Phyllodes tumors (PTs) are a type of rare biphasic breast tumors that account for less than 1% of all breast tumors. Although malignant PT with heterologous sarcomatous differentiation is already a rare occurrence, it can further present with various types of differentiation, such as rhabdomyosarcomatous differentiation. Case Report: In this report, we describe the case of a 42-year-old woman who presented with a malignant PT with rhabdomyosarcomatous differentiation, an even rarer form of this tumor. To the best of our knowledge, only four confirmed cases of this type of PT have been documented in the literature. Conclusion: Due to its rarity, the diagnosis of malignant PT with rhabdomyosarcomatous differentiation can be challenging, and prompt recognition is essential for optimal patient management. Clinicians should keep this rare entity in mind when encountering patients with biphasic breast tumors and consider thorough pathological evaluation for accurate diagnosis and timely treatment.
|
6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ffa47b390000005707000001000400 Introduction
Phyllodes tumors (PTs) are rare tumors of the breast and account for less than 1% of all breast tumors. Malignant Phyllodes tumor (MPT) accounts for only 10-30% of all Phyllodes tumors [ 1] and malignant Phyllodes tumor with heterologous sarcomatous differentiation is still rarer. Histologically malignant Phyllodes tumors may show significant heterogeneity in morphology such as angiosarcoma, lipo-sarcomatous, fibrosarcomatous, chondro-sarcomatous, rhabdomyo-sarcomatous, or osteo-sarcomatous differentiation [ 2]. Proper histopathological diagnosis and subtyping of the sarcomatous components are essential for deciding the correct treatment and prognosis of patients with MPT. MPTs with rhabdomyosarcomatous differentiation are scarcely seen with only four confirmed cases documented till date to the best of the knowledge after a thorough search of literature [ 3]. Herein we present the case of a 42 years old woman with a breast malignant PT with rhabdosarcomatous differentiation.
Case Report
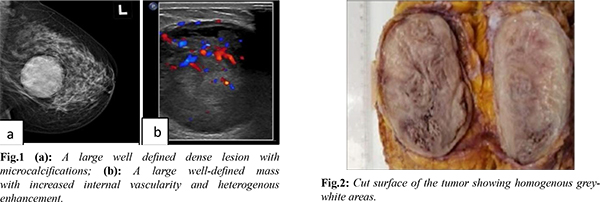
A 42-year-old woman was admitted with a hard painful lump in left breast which had enlarged within two months. She had no past history of malignancy and no history of prior irradiation to the breast or chest region. She gave history of excision of left breast fibroadenoma 23 years back. Physical examination indicated a 6×6 cm hard mass located in the upper outer and middle quadrants of the left breast. The axillary lymph nodes were not palpable. Mammographically, a large well defined dense lesion with associated microcalcifications was noticed [Fig.1a]. CT scan showed a large well-defined mass in the left breast with increased internal vascularity and heterogenous enhancement [Fig.1b]. A left modified radical mastectomy with axillary clearance level was performed. The specimen handled at the pathology laboratory was 26×25×6 cm in size. Series sections of the specimen showed a well-circumscribed firm to hard solid tumor mass measuring 8.5×6×5 cm, with a bosselated cut surface in a leaf-like pattern and necrosis [Fig.2]. The surgical margins of the resection were free of the tumor.
Microscopically, multiple hematoxylin and eosin-stained slides of the tumor revealed a biphasic tumor with spindled tumor cells proliferating in fascicles and displaying moderate to marked nuclear atypia with high mitotic rate 12/10 hpf. Heterolo-gous rhabdomyosarcomatous differentiation was noted. No necrosis was observed [Fig.3a-d]. The cells express SMA diffusely while Desmin, Myogenin and MyoD1 are strongly positive in the areas of rhabdomyosarcomatous differentiation. Tumor cells were immunonegative for CD34, BCL2, PanCK, p63, ER, CD117, PR, Her2neu. Based on morphologic and immunohistochemical insignia, the case was diagnosed as a ‘malignant Phyllodes tumor of the breast with rhabdosarcomatous differentiation’. Evidence of the lymph node metastasis or a systemic spread following total surgical excision of the tumor was not found, and close follow-up was recommended.
Discussion
Phyllodes tumors (PTs) are rare biphasic tumors of the breast and account for less than 1% of all breast tumors. Malignant PT arises in woman in their 40’s, with the majority of cases between 35 to 55 years old. Phyllodes tumors, first described as cytosarcoma Phyllodes by Muller in 1838 [ 4], display a wide range of clinical, histological and cytological features [ 5, 6]. The term "sarcoma" was initially used because of its fleshy appearance, a more modern term is Phyllodes tumor (PT). The presence of dual population of both epithelial and stromal cells is necessary for the diagnosis of PT [ 4]. Based on atypia, mitotic activity or overgrowth in the stroma, PTs can be classified by histopathological features as benign, borderline or malignant [ 7]. Although the histological appearances of PTs are relatively poor predictors of their behavior, all PTs have the potential to become malignant [ 4]. Phyllodes tumor can only be found in mammary tissue and on histology they have a component of epithelial as well as metaplastic mesenchymal origin [ 5]. PTs are interpreted as a continuum of the spectrum of fibroepithelial neoplasms of breast tissue; benign PTs can be difficult to distinguish from fibroadenomas while malignant PTs can grow in size quickly and metastasize early [ 6]. The metastatic spread of malignant PT is mainly hematogenous to lung, with infrequent lymphatic involvement, hence axillary lymph nodes are not palpable at presentation in most cases [ 8]. The characteristic histological features are related to the stroma and PTs are differentiated from fibroadenomas by marked stromal overgrowth and hypercellularity [ 6]. Malignant Phyllodes tumors may show significant heterogeneity in morphology such as angiosarcoma, lipo-sarcomatous, fibrosarcomatous, chondro-sarcomatous, rhabdomyo-sarcomatous, or osteo-sarcomatous differentiation [ 2]. Marked fibrosarcomatous changes of the stromal component are seen with the epithelial component being absent/negligible. A thorough search of literature shows that heterologous sarcomatous transformation towards liposarcoma, fibrosarcoma, angiosarcoma, osteosarcoma, chondrosarcoma, osteoclast like giant cells and rhabdomyosarcoma have been occasionally encountered in the said order of frequency. Recent literature suggests that liposarcoma as a heterologous component is no longer a histological criterion of malignancy, because atypical adipocytes in liposarcoma do not harbour MDM2 aberrations or CDK4 amplification. Primary rhabdomyosarcomas (RMS) occurring in breast are also exceedingly rare, mostly present as metastasis from other sites. Genetic abnormalities associated with Phyllodes tumors are loss of nuclear Beta-Catenin, amplification of MYC and aberrant expression of TP53. Other described cytogenetic changes seen specifically in the malignant ones include gain in chromosome 1q and losses at chromosome 13 [1]. The prognosis of Phyllodes tumor is quite good. The five-year survival rate for malignant Phyllodes tumors was 82% [9]. In 15% of cases, PT will locally recur [10]. Treatment of MPTs is complete surgical excision with wide clear margins of at least 1 cm. Unlike primary rhabdomyosarcoma, where adjuvant radiation therapy/chemotherapy are beneficial, their role in MPTs with rhabdomyosarcomatous differentiation is not very well known because of the rarity of such cases [1].
Conclusion
Our findings showed that diagnosis of this tumor should be performed using a combination of clinical, pathological, and immunohistochemical staining results. The main treatment for malignant PT is extensive local resection or total mastectomy.
Contributors: SP, ST: Histopathology, data acquisition and drafting of the manuscript; MAM, SSP: histopathology and critical inputs into the manuscript. SP will act as a study guarantor. All authors approved the final version of this study and are responsible for all aspects of the study. Funding: None; Competing interests: None stated.
References - Yadav K, Malignant Phyllodes tumour with rhabdomyosarcomatous differentiation: A rare phenomenon. Journal of Clinical & Diagnostic Research. 2021;15:4-6.
- Rosen PP. Fibroepithelial neoplasms. In: Rosen PP, editors. Rosen's Breast Pathology. 3rd ed. Philadelphia: Lippincott Williams and Wilkins; 2009: p. 208-209.
- Lakhani SR, Ellis IO, Schnitt SJ, Tan PH, van de Vijver MJ [eds]. World Health Organization [WHO] Classification of tumours of the breast. WHO Classification of Tumours, 4th edition, vol. 4, International Agency for Research on Cancer [IARC] Press, Lyon, France, 2012: p. 143-147.
- Fiks A. Cystosarcoma Phyllodes of the mammary gland–Muller’s tumor. For the 180th birthday of Johannes Muller, Virchows Archiv A Pathol Anat Histol. 1981;392:1-6.
- Al-Zoubaidi M, Qiu S, Bonnen M, Joyner M, Roehl K, Silva C, et al. Malignant Phyllodes tumor of the breast: a case report. The Open Breast Cancer Journal. 2011;3:45-48.
- Parker SJ, Harries SA. Phyllodes tumours. Postgrad Med J. 2001;77:428-435.
- Telli ML, Horst KC, Guardino AE, Dirbas FM, Carlson RW. Phyllodes tumors of the breast: natural history, diagnosis, and treatment. J Nat Compr Cancer Netw. 2007;5:324-330.
- Nayak M, Patra S, Mishra P, Sahoo N, Sasmal PK, Mishra TS, et al. Malignant Phyllodes tumour with heterologous differentiation: Clinicopathological spectrum of nine cases in a tertiary care institute in Eastern India. Indian J Pathol Microbiol. 2017;60:371-376.
- Chaney AW, Pollack A, McNeese MD, Zagars GK, Pisters PW, Pollock RE, et al. Primary treatment of cystosarcoma Phyllodes of the breast. Cancer. 2000;89:1502-1511.
- Barth RJ Jr, Wells WA, Mitchell SE, Cole BF. A prospective, multi-institutional study of adjuvant radiotherapy after resection of malignant Phyllodes tumors. Ann Surg Oncol. 2009;16:2288-2294.
|