6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ffe49a390000005707000001000500
Introduction
Choriocarcinoma is a rare but aggressive form of cancer that arises from trophoblastic cells, which are responsible for the formation of the placenta during pregnancy. It can develop after any type of pregnancy, including miscarriage, ectopic pregnancy, molar pregnancy, or full-term delivery. Choriocarcinoma is one of the types of Gestational Trophoblastic Disease (GTD), a group of disorders that result from abnormal growth of trophoblastic cells. The incidence of GTD is approximately 1 in 1000 pregnancies, with choriocarcinoma accounting for about 15% of cases of GTD worldwide. However, choriocarcinoma is more common in certain regions such as Asia and Africa, where the incidence rate can reach up to 8 per 100,000 pregnancies [
1].
Choriocarcinoma is known to present diagnostic challenges due to its varied clinical manifestations. The most common presenting symptom is vaginal bleeding, which can be heavy and prolonged, and may be accompanied by abdominal pain and/or an enlarged uterus. However, other symptoms such as nausea, vomiting, fatigue, and respiratory distress can also occur. The diagnosis of choriocarcinoma is based on a combination of clinical features, imaging studies, and laboratory tests. In particular, measurement of serum beta human chorionic gonadotropin (ß-HCG) levels is essential for the diagnosis and management of GTD, as ß-HCG levels are elevated in nearly all patients with choriocarcinoma.
Delayed diagnosis of choriocarcinoma can result in significant morbidity and mortality, as the tumor can metastasize rapidly to distant sites such as the lungs, liver, and brain. Therefore, a high degree of suspicion for GTD should be kept in mind when evaluating women with abnormal uterine bleeding following any obstetric event, and prompt testing with urine pregnancy test and ß-HCG estimation should be performed if indicated [2,3].
Case Report
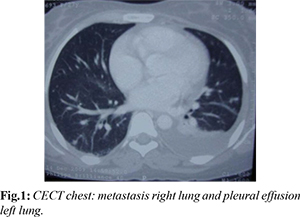
A 26-year-old woman (para 2, live 2, abort 1) presented in medical emergency with complaints of breathlessness for 1 month, orthopnea, and distension abdomen for 5 days. She was found to be in a state of shock with vital parameters of pulse 126/minute, BP systolic 80 mmHg, and RR 26/minute. On examination, distension abdomen and presence of free fluid were observed. Shock was managed with intravenous fluids, packed cell volume, fresh frozen plasma (FFP), and dopamine infusion. An ultrasound of the abdomen revealed a bulky uterus with multiple hypoechoic masses in the anterior wall and a heterogeneous endometrial echo with multiple cystic lesions. Bilateral multi-septate cystic ovaries were also observed. Ultrasound-guided paracentesis revealed frank blood, and the patient was referred to gynecology emergency. CECT chest revealed presence of metastasis in lung and presence of pleural effusion on left side [Fig.1].
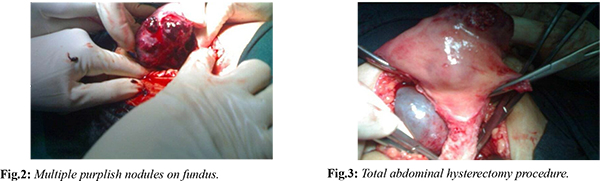
The patient had a history of spontaneous abortion 9 months back, following which she had complaints of irregular bleeding per vaginum off and on since then. She attended another hospital twice in the past 9 months for similar complaints, where she was diagnosed as a case of incomplete abortion with severe anemia, and dilatation & curettage (D&C) was done on both occasions. She also received packed cells on both occasions, and except for complete blood count, no other investigations were done in the previous hospital. On examination in gynecology emergency, except for tachycardia, no other abnormality was detected. A provisional diagnosis of hemoperitoneum leading to shock secondary to Gestational Trophoblastic Neoplasia was made. Urine pregnancy test (UPT) was positive, and beta HCG was highly raised. The patient was taken up for emergency exploratory laparotomy, which revealed the presence of approximately 2.0 liters of hemoperitoneum and multiple purplish colored nodules on the uterine fundus. The decision for total abdominal hysterectomy was taken, and bilateral decompression of theca lutein cysts was done [Fig.2-4]. Thorough peritoneal lavage was done, and 4 units of packed cells and 2 units of FFP were transfused intra-operatively.

In the post-operative period, the patient remained on ventilatory support for 2 days and on inotropes for 5 days. The patient was given another 4 packed cells, 2 FFP, and 2 units of platelet concentrate. Specimen analysis revealed it as choriocarcinoma involving the full thickness of the uterus and extending through the serosa [Fig.5]. The final diagnosis of Gestational Choriocarcinoma stage 3 with WHO risk score 10 was made. Adjuvant combination chemotherapy EMA-CO regimen for 6 cycles was given to the patient, and the patient recovered by the 18th postoperative day.
Discussion
Gestational Trophoblastic Neoplasia (GTN) is a rare gynecologic malignancy that arises from the abnormal proliferation of trophoblastic cells, which are the cells that form the placenta during pregnancy. The most common types of GTN are hydatidiform mole, invasive mole, choriocarcinoma, placental site trophoblastic tumor, and epithelioid trophoblastic tumor. Choriocarcinoma is the most malignant form of GTN, and it can occur following any type of pregnancy, including a normal pregnancy, a miscarriage, or an ectopic pregnancy [
4].
The incidence of GTN varies between regions, with the highest rates reported in Asia, particularly in Indonesia, the Philippines, and Thailand. In India, the incidence of GTN has been reported to be between 1.4 and 1.7 per 1,000 live births [5]. GTN can present with a wide range of symptoms, depending on the type and extent of the disease. Common symptoms include abnormal vaginal bleeding, pelvic pain or pressure, and an enlarged uterus [4]. The case report presented here highlights the rare presentation of choriocarcinoma as a uterine perforation and hemoperitoneum. The delay in diagnosis and initial mismanagement of the patient's symptoms likely contributed to the severity of her condition upon presentation to the medical emergency department. It is recommended to evaluate prolonged bleeding following any obstetric event thoroughly, and UPT and beta HCG estimation should be done in each and every case. All curettage following D&C needs histopathological analysis. The importance of early diagnosis and management of GTN cannot be overstated, as delayed diagnosis can lead to poor outcomes and increased morbidity.
The management of GTN typically involves surgical intervention and chemotherapy. The surgical approach depends on the type and extent of the disease, but it often involves a hysterectomy with or without removal of the ovaries. Chemotherapy is typically administered following surgery, and the choice of chemotherapy regimen depends on the stage and risk score of the disease [4].
Conclusion
GTN is a rare but potentially life-threatening gynecologic malignancy that can present with a wide range of symptoms. Early diagnosis and management are crucial to improve outcomes and reduce morbidity. Clinicians should maintain a high index of suspicion for GTN in patients with prolonged bleeding following any obstetric event, and they should be aware of the potential for rare presentations such as uterine perforation and hemoperitoneum.
Contributors: PL, SD: manuscript writing, patient management; TDS, KA, MP: manuscript editing, patient management; RL: surgery and critical inputs into the manuscript. PL will act as a study guarantor. All authors approved the final version of this manuscript and are responsible for all aspects of this study.
Funding: None; Competing interests: None stated.
References
- Seckl MJ, Sebire NJ, Berkowitz RS. Gestational trophoblastic disease. Lancet. 2010;375(9721):717-729.
- Tidy JA, Rustin GJ. The management of patients with gestational trophoblastic neoplasia. Semin Oncol. 1995;22(3):216-223.
- Lybol C, Sweep FC, Harvey R, Mitchell H, Short D, Thomas CM, et al. Diagnosis and treatment of gestational trophoblastic disease: A multidisciplinary update. Int J Gynecol Cancer. 2014;24(8):S53-61.
- Lurain JR. Gestational trophoblastic disease I: epidemiology, pathology, clinical presentation and diagnosis of gestational trophoblastic disease, and management of hydatidiform mole. Am J Obstet Gynecol. 2010;203(6):531-539.
- Gupta S, Gupta N, Singh S. Gestational trophoblastic disease: A 10-year study of patients treated at a tertiary care center in India. J Reprod Med. 2012;57(5-6):205-210.