|
Mario Vetrano1,3, Maurizio Taurino2,3, Flavia Santoboni1,3, Serena Michelini1,3, Andrea Ruggieri1,3, Claudia Maggiore2,3, Eleonora Latini1,3, Sveva M. Nusca1,3, Maria C. Vulpiani1,3 1Unit of Physical Medicine and Rehabilitation, Department of Medical Surgical Sciences and Translational Medicine and 2Unit of Vascular Surgery, Department of Clinical and Molecular Medicine, "Sapienza" University of Rome, Italy; 3Sant'Andrea University Hospital, Via di Grottarossa 1035, 00189 Rome, Italy.
Corresponding Author:
Dr. Flavia Santoboni Email: flavia.santoboni@gmail.com
Abstract
Background: Intermittent claudication (IC) is a common symptom of Peripheral Artery Disease (PAD) mostly caused by arterial stenosis and/or occlusion in the lower extremities, typically resulting from atherosclerosis. Although less frequent, congenital vascular malformations and thromboangiitis obliterans, also known as Buerger’s disease (BD), can also cause IC, leading to progressively worsening symptoms, especially during walking. Extracorporeal Shock Wave Therapy (ESWT) is a non-invasive treatment that has been studied for its potential to promote neovascularization and vasodilation in PAD. Case Report: We present a man with congenital bilateral deep femoral artery agenesis and concomitant BD who underwent ESWT of the leg muscles. The treatment significantly improved his walking abilities, alleviated pain, and enhanced his quality of life, which persisted even 18 months after treatment. Conclusion: Functional and clinical improvements, in addition to quality of life, suggest that ESWT could represent a promising symptomatic treatment for PAD.
|
6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ff24ba390000003b0c000001000100 Introduction
Among the causes of intermittent claudication, there are congenital vascular malformations and thromboangiitis obliterans, also known as Buerger’s disease (BD). We present the case of a patient with congenital bilateral deep femoral artery agenesis and concomitant BD that achieved an improvement in walking abilities, pain and quality of life after the treatment of the leg muscles with Extracorporeal Shock Wave Therapy (ESWT).
Case Report
A 46-year-old man, with no other relevant diseases, but heavy smoker for more than 30 years, came to our observation in September 2015 for referred claudication, increasing progressively in recent months, up to a very short walking ability (less than 100 mt.), more significantly on the left lower limb. Once neurological and musculoskeletal pathologies were excluded, the patient underwent CT angiography of the vessels of the lower limbs which showed on the left side: agenesis of the deep femoral artery, of the anterior tibial and of interosseous arteries, and occlusion of the superficial femoral artery; on the right side, agenesis of the deep femoral artery, occlusion of the anterior and posterior tibial arteries and interosseous artery [Fig.1].

Besides gradually smoking cessation, following the diagnosis of BD, the patient first underwent bilateral lumbar chemical sympatholysis to control pain, then recanalization with multilayer Supera® (5×200 mm) stenting of the left superficial femoral artery and percutaneous transluminal angioplasty (PTA) with Drug-eluting balloon (DEB) (Elutax 4 x 100 mm) for the tibio-peroneal trunk. Moreover, the patient was submitted to Iloprost® infusion (Iloprost 0.05 mg/0.5 mL), repeated every 6-8 months from November 2016 until October 2018. The infusion therapy was performed in a day hospital setting, 5 times per week, for 2 weeks. According to current guidelines [1], he took dual antiplatelet treatment (acetylsalicylic acid 100 mg and clopidogrel 75 mg, once a day). Additionally, pentoxifylline 400 mg, three times a day, was administered. Despite these treatments, the patient complained about the persistent functional limitation in walking ability due to the pain, more important to the left side with respect to the contralateral. The tissue oxygen partial pressure values were lower on the left side compared to the right side, with the anterior tibial muscle measuring 27 mmHg versus 42 mmHg (right), posterior tibial muscle measuring 54 mmHg versus 82 mmHg (right), lateral gastrocnemius measuring 68 mmHg versus 89 mmHg (right), and medial gastrocnemius measuring 69 mmHg versus 89 mmHg (right). These findings confirmed the presence of referred symptoms. For this reason, in January 2019, we decided to treat the patient with a cycle of focalized ESWT only on the left lower limb, during which the patient has only continued the dual antiaggregant therapy and the pentoxifilline. The treatment consisted of 8 sessions performed twice a week for 4 weeks. In each session, lasting about 20 minutes, 5000 pulses of shock waves (at 4 Hz and an energy flux density of 0.07-0.15 mJ/mm²) were delivered in the left leg to the calf muscle bulk, divided into 1500 pulses on each head of the gastrocnemius muscle and 2000 impulses on soleus muscle, according to previous studies [ 2, 3]. A Modulith® SLK shockwave device (Storz Medical AG, Switzerland) was used. Before ESWT (T0) and 1 (T1), 3 (T2), 6 (T3) and 18 (T4) months after the treatment, instrumental and functional parameters were assessed. Furthermore, at the last follow up the patient underwent CT angiography of the vessels of the lower limbs [Fig.2].
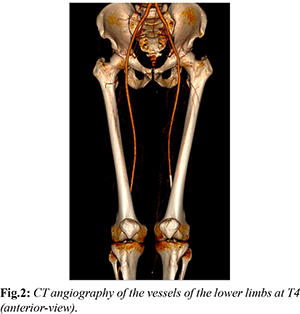
In particular, instrumental parameters like Ankle Brachial Index (ABI) and Tissue Oxygen partial pressure (t-pO2) at the anterior and posterior tibial muscles and medial and lateral gastrocnemius have been determined. Functional parameters were Pain Free Walking Distance (PFWD) and Maximum Walking Distance (MWD) measured on a treadmill at 2.5 km/h with a 10-degree incline to a maximum of 10 minutes, supervised by the same medical doctor. Finally, the quality of life has been evaluated by the EQ-5D questionnaire. The patient gave his written informed consent to the treatments and the permission to release his personal and clinical data for publication. During the follow-up period, the patient referred improvement in both walking ability and quality of life. The PFWD data of the treated side showed a positive trend starting from the first month after treatment, with a value at the last follow-up 64.3% higher than the initial one. Similarly, MWD was also increased one month after the treatment (35.3%), and the value remained almost unchanged (29.4%) at the 18-month follow-up [Table 1]. The data of the EQ-5D questionnaire showed an overall improvement of the quality of life, during the follow up [Table 2]. No substantial differences were detected in the others clinical and instrumental parameters assessed. CT angiography at 18 months after the treatment showed complete stent occlusion of the left superficial femoral artery [Fig.3].
Discussion
The patient, in the present clinical case, was suffering from both congenital vascular malformation and BD, so that the concomitant diseases could, in part, justify the unsatisfactory control of symptoms with the conventional therapy. Vascular congenital malformations involving iliac and femoral vessels are rare. In a previous study including 8000 angiograms, only 6 cases of aortoiliac and iliofemoral variations were found [ 4]. BD is a non-atherosclerotic segmental inflammatory disease that affects the small and medium-sized arteries and veins, both in the upper and lower extremities, in many cases without possibility of revascularization [5]. Recent studies have suggested that ESWT is a novel, safe, non-invasive and effective treatment for peripheral arterial disease (PAD) [3,6]. The mechanisms by which ESWT might determine these clinical improvements remain unclear. Several studies demonstrated an increase in VEGF concentrations and VEGFR2 activation after ESWT [7,8], suggesting their possible crucial role in the formation of new vessels. Moreover, ESWT has been demonstrated to have an anti-inflammatory effect with upregulation of eNOS activity [9]. Indeed, the role of shock waves in tissue regeneration and perfusion has also been demonstrated in the treatment of other vascular diseases. In 2010, Vardi et al. first reported the use of low-intensity extracorporeal shockwave therapy (LI-ESWT) in the treatment of erectile dysfunction, indicating their physiological effects on cavernous hemodynamics [10]. Other authors have confirmed that shock waves have positive influence on the proliferation and differentiation of cardiomyocytes, smooth muscle and endothelial cells precursors, probably by the activation of VEGF/ERK/MAPK (mitogen-activated protein kinase) pathway, showing improvement of the myocardial function in patients with refractory angina patients [11]. The efficacy, safety and tolerability of the ESWT have been demonstrated in the treatment of PAD, when it was related to a single cause. BD is a chronic obliterating degenerative disease, with a progressive worsening of clinical symptoms and loss of function. In a previous study, Serizawa et al. reported positive effects of the ESWT in a patient with thromboangiitis obliterans [3]. These results encouraged us to investigate the potential role of this treatment, in addition to the conventional therapies in a subject with a double vascular disease, in order to avoid progressive worsening. Our findings showed an improvement in functional limitation, demonstrated by the increasing of PFWD and MWD, and in quality of life highlighted by EQ-5D questionnaire. No changes were found in ABI and t-pO2 suggesting that the angiogenic response to ESWT is probably obtained mainly at the microvascular level rather than on the macro circulation, as Harwood and co-workers speculated in 2018 [2]. These data confirm the action of shock wave as a drive of neo-angiogenesis, resulting in an improvement of tissue perfusion. In fact, since BD affects the small vessels and the mechanism of action of the shock waves seems to influence the microcirculation rather than the macro-circulation, this observation could justify its positive effect in the treatment of claudication. The major clinical improvement in PFWD, MWD values and in the quality of life was observed at last follow up. It could be justified by the peculiarity of the conditions of the patient, affected by both a congenital vascular anomaly and a progressive vascular occlusive pathology and, furthermore, it could derive from the biological time needed for the development of new micro-vessels. It is noteworthy that from October 2019 to June 2020, Iloprost® infusion was no longer necessary due to the considerable reduction of pain symptoms, and it could be explained as an additional positive effect of shock wave treatment. Moreover, despite the stent occlusion highlighted at the last follow-up and without any modification of the pharmacological therapies, the patient showed clinical and functional improvement, and this could be justified even more by shock wave treatment. In the present case, ESWT resulted not only an effective, non-invasive and painless alternative treatment in PAD but also less expensive and time consuming than Iloprost therapy alone.
Conclusion
Despite the complex underlying diseases of the patient, ESWT determined an improvement in his symptoms and quality of life and, for this reason, it could represent an innovative treatment in selected conditions that cause intermittent claudication. Although further experimental studies and large-scale clinical trials are needed, ESWT remains a promising alternative therapy for PAD.
Contributors: MV, MT: Contributed data or analysis tools, performed the analysis, manuscript writing; FS: corresponding author, conceived and designed the analysis; contributed data or analysis tools; manuscript writing; SM, AR: performed the treatment, contributed data or analysis tools, performed the analysis; collected the data; literature review; CM, EL, SMN, MCV: contributed data or analysis tools; performed the analysis; collected the data, manuscript editing. Funding: None; Competing interests: None stated.
References - Gerhard-Herman MD, Gornik HL, Barrett C, Barshes NR, Corriere MA, Drachman DE, et al. 2016 AHA/ACC guideline on the management of patients with lower extremity peripheral artery disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2017;135:e686-e725.
- Harwood AE, Green J, Cayton T, Raza A, Wallace T, Carradice D, et al. A feasibility double-blind randomized placebo-controlled trial of extracorporeal shockwave therapy as a novel treatment for intermittent claudication. J Vasc Surg. 2018;67:514-521.
- Serizawa F, Ito K, Kawamura K, Tsuchida K, Hamada Y, Zukeran T, et al. Extracorporeal shock wave therapy improves the walking ability of patients with peripheral artery disease and intermittent claudication. Circulation Journal. 2012;76:1486-1493.
- Greebe J. Congenital anomalies of the iliofemoral artery. J Cardiovasc Surg. 1977;18:317-323.
- Olin JW, Shih A. Thromboangiitis obliterans (Buerger’s disease). Curr Opin Rheumatol. 2006;18:18-24.
- Cayton T, Harwood A, Smith GE, Chetter I. A systematic review of extracorporeal shockwave therapy as a novel treatment for intermittent claudication. Annals of Vascular Surgery. 2016;35:226-233.
- Holfeld J, Tepekoylu C, Blunder S, Lobenwein D, Kirchmair E, Dietl M, et al. Low energy shock wave therapy induces angiogenesis in 300 acute hind-limb ischemia via VEGF receptor 2 phosphorylation. PloS one. 2014;9:e103982.
- Oi K, Fukumoto Y, Ito K, Uwatoku T, Abe K, Hizume T, et al. Extracorporeal shock wave therapy ameliorates hindlimb ischemia 306 in rabbits. Tohoku J Exp Med. 2008;214:151-158.
- Ito K, Fukumoto Y, Shimokawa H. Extracorporeal shock wave therapy for ischemic cardiovascular disorders. Am J Cardiovasc Drugs. 2011;11:295-302.
- Vardi Y, Appel B, Jacob G, Massarwi O, Gruenwald I. Can low-intensity extracorporeal shockwave therapy improve erectile function? A 6-month follow-up pilot study in patients with organic erectile dysfunction. Eur Urol. 2010;58:243-248.
- Li H, Liu ML. Cardiac shock wave therapy: an alternative non-invasive therapy for refractory angina. Eur Rev Med Pharmacol Sci. 2018;22:5402-5410.
|