Introduction
Pulmonary metastasis to the breast has an incidence of 0.5-3% [
1]. These patients often present with symptoms that resemble primary breast cancer, and it can be difficult to differentiate them clinically. Since management and prognosis for primary and secondary breast cancers differ significantly, making an accurate diagnosis is crucial. This not only ensures that patients receive the appropriate treatment but also maximises their outcomes.
Case Report
A 61-year-old lady was found to have a new right breast lesion in 2021 on her yearly surveillance imaging for a previous T2N1M0 left breast cancer diagnosed in 2017. It was a grade 3, oestrogen receptor (ER) positive, progesterone receptor (PR) positive and human epidermal growth factor receptor 2 (HER2) negative invasive ductal carcinoma. Breast-conserving surgery with sentinel lymph node biopsy was performed, followed by level II axillary clearance. She also received adjuvant chemotherapy, radiotherapy, and endocrine therapy. Due to significant family history of breast cancer, she was tested for breast cancer genes BRCA1 and 2, both of which were negative.
In the interim, an incidental left upper lobe lung nodule was identified when she presented to the emergency department with dyspnoea in 2020. The lesion was biopsied and the histopathology revealed a poorly differentiated adenocarcinoma with a programmed death-ligand 1 (PD-L1) expression of 60%. This stage IIIa non-small cell lung cancer (NSCLC) was treated with definitive chemoradiotherapy followed by immunotherapy. She is an ex-smoker with no significant past medical history, with Eastern Cooperative Oncology Group (ECOG) performance status 1.
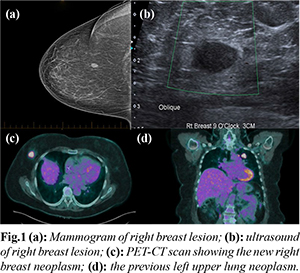
The new right breast lesion appeared as a well-circumscribed, low-density opacity on mammogram [Fig.1a]. This corresponded to a 15 mm round, hypoechoic lesion at 9 o’clock, 3 cm from the nipple on ultrasound [Fig.1b], which was reported as Breast Imaging-Reporting and Data Systems category 3 (BIRADS 3), possibly a complex cyst. No associated axillary lymphadenopathy was demonstrated. A subsequent core biopsy showed a high grade, triple-negative carcinoma. Staging positron emission tomography and computed tomography (PET-CT) scan showed a hypermetabolic right breast neoplasm with no evidence of locoregional lymph node or distant metastatic disease [Fig.1c]. At the same time, the pulmonary neoplasm was noted to have substantially decreased in size and metabolic activity [Fig.1d].
In the setting of previous contralateral breast cancer being of favourable pathology with positive ER/PR without evidence of genetic mutation, the new development of an aggressive triple negative breast cancer raised the possibility that this could be a metastatic lesion in light of concurrent pulmonary cancer burden. The histopathology of the new right breast lesion and previous lung biopsy were subsequently reviewed in a multidisciplinary meeting, with further immunohistochemical staining performed.
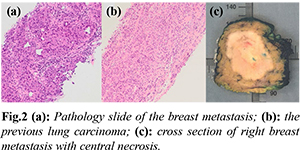
The morphology and immuno-histochemistry of the two shared similar pathological profiles [Fig.2a and 2b]; they were positive for lung cancer markers cytokeratin (CK) 7, 8 and 18 and negative for ER and PR [2]. However, the expression of immunohistochemical markers become less reliable with more poorly differentiated tumors [3]. Therefore, further molecular testing was performed to help establish the final diagnosis of a metastatic disease where KRAS mutation was demonstrated in both lesions. KRAS is a proto-oncogene frequently encountered in lung, colorectal and pancreatic cancers [4]. Given that the patient had a solitary metastasis to the breast with good treatment response to the primary lung cancer, she underwent a hookwire-localised wide local excision of the breast metastasis. Intra-operatively, the mass had become palpable within the 30-day booking category, demonstrating its rapid growth. The final histopathology confirmed complete excision of a 43 mm poorly differentiated carcinoma with central necrosis and lymphovascular invasion [Fig.2c]. She is currently continuing with immunotherapy, Durvalumab.
Discussion
Metastatic disease to the breast from lung adenocarcinomas is challenging to diagnose as they have features that closely mimic triple-negative breast cancers. It often presents as a painless, well-circumscribed solitary mass with predilection to the upper outer quadrant [
5,
6]. Despite its superficial location, skin or nipple changes are rare. In contrast to primary breast cancers, the characteristic calcification and spiculation on mammogram are uncommon [
7]. Although immunohistochemistry plays a crucial role in identifying the primary origin of cancers in the setting of unusual cytology, poorly differentiated cancers like metastases are associated with lower levels of tumor marker expression [
3]. Since these impacts on diagnostic accuracy, further molecular testing should be considered before making a clinical decision.
Despite advancements in treatment, stage IV NSCLC carries a poor prognosis, with an estimated 1-year mortality of over 80% [1]. Therefore, the treatment intent is palliative, with the recommended MDT approach entailing conservative surgical intervention with wide local excision of the metastasis if appropriate, along with systemic chemotherapy and radiotherapy in patients with acceptable performance [8].
Conclusion
Pulmonary metastasis to the breast is uncommon and difficult to diagnose. Clinical suspicion in unusual disease patterns remains the key to accurate diagnosis and decision making, in conjunction with knowledge on utility of available radiological and pathological investigations and pitfalls around them.
Contributors: SSWP: manuscript writing, patient management; SN: manuscript editing, patient management; RP: critical inputs into the manuscript. SSWP will act as a study guarantor. All authors approved the final version of this manuscript and are responsible for all aspects of this study.
Funding: None; Competing interests: None stated.
References
- Babu KS, Roberts F, Bryden F, McCafferty A, Downer P, Hansell DT, et al. Metastases to breast from primary lung cancer. J Thorac Oncol. 2009;4(4):540-542.
- Kanaji N, Bandoh S, Ishii T, Fujita J, Ishida T, Matsunaga T, et al. Cytokeratins negatively regulate the invasive potential of lung cancer cell lines. Oncol Rep. 2011;26(4):763-768.
- Nakamura N, Miyagi E, Murata S, Kawaoi A, Katoh R. Expression of thyroid transcription factor-1 in normal and neoplastic lung tissues. Mod Pathol. 2002;15(10):1058-1067.
- Jancík S, Drábek J, Radzioch D, Hajdúch M. Clinical relevance of KRAS in human cancers. J Biomed Biotechnol. 2010;2010:150960.
- Williams SA, Ehlers II RA, Hunt KK, Yi M, Kuerer HM, Singletary SE, et al. Metastases to the breast from nonbreast solid neoplasms. Cancer. 2007;110(4):731-737.
- Toombs BD, Kalisher L. Metastatic disease to the breast: clinical, pathologic, and radiographic features. Am J Roentgenol. 1977;129(4):673-676.
- Wang L, Wang SL, Shen HH, Niu FT, Niu Y. Breast metastasis from lung cancer: a report of two cases and literature review. Cancer Biol Med. 2014;11(3):208-215.
- Vaughan A, Dietz JR, Moley JF, Debenedetti MK, Aft RL, Gillanders WE, et al. Metastatic disease to the breast: the Washington University experience. World J Surg Oncol. 2007;5:74.