Introduction
Osteochondritis dissecans (OCD) of the knee is an uncommon condition, particularly in elderly individuals, with an estimated incidence of approximately 3 in 100,000 individuals [
1]. OCD affects subchondral bone and the overlying articular cartilage, often presenting in weight-bearing joints such as the knee. While adolescent OCD cases, especially those with open growth plates, tend to have more favourable outcomes with conservative or minimally invasive treatment, the same cannot be said for adult presentations. Management strategies for adult OCD, particularly in elderly athletes or active individuals, remain variable and poorly defined. They range from conservative physiotherapy to more invasive approaches such as osteochondral grafting or even total knee arthroplasty (TKA), depending on the severity and activity level of the patient [
2]. This case report highlights a combined approach using Osteochondral Autograft Transplantation (OATS) and Medial Opening Wedge High Tibial Osteotomy (MOWHTO) to preserve joint function and delay or avoid the need for TKA in an active middle-aged patient with OCD and varus malalignment.
Case Report
A 51-year-old male presented to our outpatient department with complaints of mild swelling and pain in the left knee following a recent fall. Initial radiographs showed no acute bony injuries but revealed early osteoarthritic changes consistent with Kellgren-Lawrence Grade II. Conservative treatment was initiated. However, upon resolution of acute symptoms, a detailed clinical examination was performed, revealing tenderness over the medial femoral condyle and a positive Wilson’s test. The patient exhibited bilateral varus alignment (left > right) and an antalgic gait.
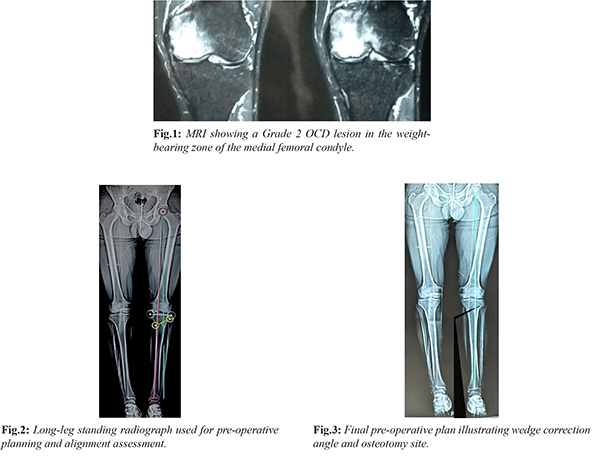
Further imaging was advised, including MRI, CT scan, and long-standing alignment radiographs. MRI revealed a Grade II OCD lesion on the medial femoral condyle (ICRS classification) [Fig.1]. CT imaging defined the lesion size as 10 mm (anteroposterior) × 8 mm (mediolateral) × 7 mm (depth), located in the weight-bearing zone of the medial femoral condyle. Long-standing radiographs using the Mikulicz line and Dror Paley method demonstrated a 9° varus deformity in the left leg. Preoperative planning with Hernigou's tables estimated a required correction height of 7 mm [Fig.2,3]. Despite structured conservative management including analgesia and physiotherapy the patient’s symptoms progressed, limiting his ability to perform activities of daily living. After appropriate counselling, the decision was made to proceed with combined Osteochondral Autograft Transplantation (OATS) and Medial Opening Wedge High Tibial Osteotomy (MOWHTO).
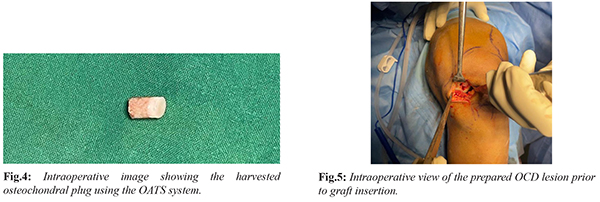
Under spinal anaesthesia, the patient was placed supine with the knee in 90° flexion using a bolster. Diagnostic arthroscopy through anterolateral and anteromedial portals identified the OCD lesion on the medial femoral condyle. Using the OATS system (COR Precision Target Cartilage Repair System – DePuy Mitek), a 10 mm osteochondral plug was harvested from the periphery of the patellofemoral joint [Fig.4]. Due to limited access arthroscopically, a mini-arthrotomy was performed to prepare the recipient site to a depth of 9 mm, followed by press-fit insertion of the graft [Fig.5]. The patient was then repositioned, and a 5 cm incision was made on the anteromedial tibia. Under fluoroscopic guidance, two 1.8 mm K-wires were placed just below the tibial tuberosity. An osteotomy was performed medial to lateral, stopping short of the lateral cortex. A wedge of 7 mm was opened using a calibrated distractor. The gap was filled with calcium sulphate bone substitute and fixed with a Tomofix plate (Synthes). Hemostasis was secured and the wound was closed.
The patient remained non-weight bearing for 4 weeks, followed by touch-toe and full weight bearing by 6 weeks. Early ROM and strengthening exercises were initiated from post-operative day one. Serial radiographs at immediate, 3, 6, and 9 months showed good graft incorporation and osteotomy healing [Fig.6,7]. Functional outcomes assessed via KOOS and NPRS scores at baseline, 2, 6, 12, and 24 months demonstrated significant improvement in pain and mobility.
Discussion
This case highlights the successful use of Osteochondral Autograft Transplantation (OATS) in combination with Medial Opening Wedge High Tibial Osteotomy (MOWHTO) as a safe, well-tolerated, and effective treatment strategy for Osteochondritis Dissecans (OCD) in the setting of varus malalignment and early osteoarthritis (OA). This approach may be particularly valuable for active elderly patients who have acute cartilage injury with preserved joint space.
Numerous fixation techniques for OCD have been described, including metal screws, bioabsorbable implants, and bone pegs. While internal fixation shows reasonable healing rates, Kocher et al. reported 84% success with internal fixation [3] metallic implants often require removal due to complications such as prominence or articular surface damage. Webb et al. observed a 50% reoperation rate due to implant-related issues [4]. Similarly, bioabsorbable screws carry the risk of breakage and failure, with Camathias et al. reporting a 23% failure rate [5]. The radiographs of our patient revealed early osteoarthritic changes consistent with Kellgren-Lawrence Grade II [6]. Compared to these methods, OATS offers several advantages, including excellent structural integrity, graft-host integration, and long-term durability. Studies have demonstrated consistently positive outcomes: Kobayashi et al. (2004) and Miura et al. (2007) both reported excellent clinical and MRI results in OCD patients treated with cylindrical autologous osteochondral grafts [
7-
8]. Alignment correction is crucial in such procedures. Persistent varus malalignment increases compartmental loading and may compromise graft uptake and longevity. High Tibial Osteotomy (HTO) alone has shown potential to delay total knee arthroplasty and promote cartilage regeneration, particularly in patients with mild OA. Combining HTO with cartilage repair procedures has been associated with enhanced outcomes, especially when limb alignment is addressed concurrently.
In this case, the use of an implant-free technique avoided the need for future implant removal, and adherence to a robust rehabilitation protocol contributed significantly to the patient’s recovery and functional improvement.
Conclusion
Combined OATS and MOWHTO offers a promising joint-preserving strategy for active elderly patients with OCD and mild varus-aligned OA. Careful clinical assessment, appropriate imaging, and correction of limb alignment are essential for surgical success. Avoiding implants minimizes the need for secondary procedures and enhances long-term outcomes.
Contributors: AD: manuscript writing, conceived the idea, patient management; VY: manuscript editing, patient management. AD will act as a study guarantor. Both authors approved the final version of this manuscript and are responsible for all aspects of this study.
Funding: None; Competing interests: None stated.
References
- Chau MM, Klimstra MA, Wise KL, Ellermann JM, Tóth F, Carlson CS, et al. Osteochondritis Dissecans: current understanding of epidemiology, etiology, management, and outcomes. J Bone Joint Surg Am. 2021;103(12):1132-1151.
- Weiss JM, Shea KG, Jacobs JC Jr, Cannamela PC, Becker I, Portman M, et al. Incidence of Osteochondritis Dissecans in adults. Am J Sports Med. 2018;46(7):1592-1595.
- Kocher MS, Tucker R, Ganley TJ, Flynn JM. Management of osteochondritis dissecans of the knee: current concepts review. Am J Sports Med. 2006;34(7):1181-1191.
- Webb JE, Lewallen LW, Christophersen C, Krych AJ, McIntosh AL. Clinical outcome of internal fixation of unstable juvenile osteochondritis dissecans lesions of the knee. Orthopedics. 2013;36(11):e1444-1449.
- Camathias C, Gögüs U, Hirschmann MT, Rutz E, Brunner R, Haeni D, et al. Implant failure after biodegradable screw fixation in osteochondritis dissecans of the knee in skeletally immature patients. Arthroscopy. 2015;31(3):410-415.
- Andriolo L, Candrian C, Papio T, Cavicchioli A, Perdisa F, Filardo G. Osteochondritis Dissecans of the knee - conservative treatment strategies: A systematic review. Cartilage. 2019;10(3):267-277.
- Kobayashi T, Fujikawa K, Oohashi M. Surgical fixation of massive osteochondritis dissecans lesion using cylindrical osteochondral plugs. Arthroscopy. 2004;20(9):981-986.
- Miura K, Ishibashi Y, Tsuda E, Sato H, Toh S. Results of arthroscopic fixation of osteochondritis dissecans lesion of the knee with cylindrical autogenous osteochondral plugs. American Journal of Sports Medicine. 2007;35(2):216-222.