Subrata Chakrabarti, Koushik Pan
From the Department of General Medicine, Institute of Post Graduate Medical Education & Research (S.S.K.M. Hospital), Kolkata-700020, West Bengal, India.
Corresponding Author:
Dr. Subrata Chakrabarti
Email: subratachakrabarti2011@gmail.com
Abstract
Acromegaly is a relatively uncommon endocrinology disease which can cause hypertension, atherosclerosis and heart failure. Echocardiography usually reveals the presence of cardiomyopathy often called as acromegalic cardiomyopathy. Clinically evident heart failure as a presenting manifestation in acromegalics is an uncommon presentation. We report a case of a 40 year old female with features of acromegaly that came to medical attention due to congestive cardiac failure.
|
6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ff18d105000000c202000001000700 6go6ckt5b5idvals|333 6go6ckt5b5|2000F757Tab_Articles|Fulltext Introduction
Acromegaly is an anterior pituitary disorder usually caused by a growth hormone (GH) secreting pituitary adenoma, which leads to increased production of insulin-like growth factor (IGF-1). It is a chronic and slowly developing disease, clinically progressive disfigurements or disabilities may go unnoticed at first, and diagnosis can be delayed [1]. Cardiovascular changes including hypertension and atherosclerosis are established complications of acromegaly which often lead to heart failure [2]. Cardiovascular diseases are the most common cause of death in acromegaly. The fact that the duration between diagnosis and the onset of the disease is long and that the prognosis is often dismal increases the importance of early diagnosis. Here we describe a case of acromegaly in a 40 year old woman who presented with congestive heart failure.
Case Report
A 40 year old female from rural India presented to the outpatient department with complaints of dyspnoea and palpitations for last 2 months. Dyspnoea was rapidly progressive and she was experiencing dyspnoea even at rest for last 7 days. She also had paroxysmal nocturnal dyspnoea, bipedal swelling, and cough with pink, frothy sputum for the same duration. She gave a history of progressive increase in the size of her hands and feet, excessive oiliness of the skin for last 2 years. At the same time, she noticed a gradual increase in the size of her breasts and cessation of menstrual flow. She also complained of a gradual deterioration of her vision and was unable to recognize distant objects for last 5 months. Apart from this, she suffered from severe pain in the weight-bearing joints with easy fatigability for last 8 months. She was diagnosed with stage 1 hypertension 1 year ago and she was on irregular anti-hypertensive therapy. However, she was not a known diabetic. On examination, she was found to be overweight having a body mass index of 28.7 kg/m2, with hyperpigmented oily skin and prominent supraorbital ridges and zygomatic arches. She had spade-like hands [Fig.1] and feet with increased heel-pad thickness of 25 mm [Fig.2]. She also had pitting bipedal edema and swollen non-tender breasts with expressive galactorrhea. Her pulse rate was 116 bpm, regular, but of low volume. Supine blood pressure was 110/76 mm Hg, with a faintly palpable apex beat. S1 was soft, S2 was normal, and S3 gallop with a mitral regurgitation murmur was noted. Tender hepatomegaly was present. Bilateral basal crepitation’s were present in the chest and nervous system examination showed bitemporal hemianopia.

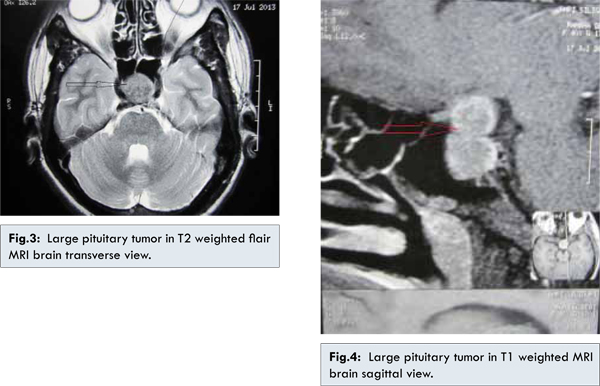
Investigations showed normocytic, normochromic anaemia with normal renal and liver function tests and normal serum electrolytes. Chest radiograph showed cardiomegaly with evidence of heart failure. Electrocardiography (ECG) showed left ventricular hypertrophy (LVH). Echocardiography revealed dilated cardiomyopathy with grade 2 diastolic dysfunction, and ejection fraction of 32%. Fasting GH level was 118 ng/mL (Normal 0.5 to 5.0 ng/mL) and IGF-1 level was 788 ng/mL (age-adjusted IGF-1 normal levels 80-500 ng/mL). On oral glucose administration test, the growth hormone values remained elevated at constant baseline level. Other hormonal evaluation revealed T3: 0.36 (0.45–1.5 ng/mL), T4: 7.6 (4.5–10 µg/mL), TSH: 1.36 (0.5–4.5 mIU/mL), FSH: 1.7 (4–14 mIU/mL), LH: 0.6 (1–18 mIU/mL), PRL: 78 (1.5–20 ng/mL). MRI brain revealed a large pituitary tumor with surrounding compression [Fig.3,4]. Final diagnosis was made as a case of acromegaly complicated by congestive heart failure. She was treated on the standard lines of management of hypertensive heart failure with intravenous furosemide and nitroglycerine infusion. She was later shifted to oral ramipril, spironolactone and hydrochlorthiazide. She was discharged with advice to attend Neurosurgery department for possible excision of the tumor.
Cardiomyopathy in acromegaly can result from structural and functional abnormalities, which may be partially reversed by effective reduction in GH and IGF-1 levels [2]. Increased frequencies of systemic hypertension and premature coronary artery disease have also been described [3]. The index patient was suffering from systemic hypertension for stage 1 hypertension for past 1 year. Studies in acromegalic cardiomyopathy have shown myocardial hypertrophy with interstitial fibrosis, lympho-mononuclear infiltration, and areas of monocyte necrosis resembling myocarditis. Increased left ventricular mass and concentric hypertrophy is also seen [4]. However, myocardial biopsy was not done in our case for want of facilities. Left ventricular hypertrophy occurs first, often leading to slow deterioration of diastolic function early in the disease [5,6].
Our index patient showed evidence of LVH with diastolic dysfunction grade 2 on ECG and echocardiography. Clinically evident congestive heart failure may develop when the disease is untreated or unsuccessfully treated [6]. Our case was also undiagnosed and untreated for 2 years which might have accelerated her heart ailments. Echocardiographic findings consist of increase in end-systolic and end-diastolic dimensions, reduction in the ejection fraction and fractional shorting, and reversal of the E/A ratio, in the presence of severe signs of congestive heart failure [7]. These echocardiographic features have often been documented in young acromegalics without any clinical evidence of cardiac impairment [8]. In our case, diminution of ejection fraction with increased end systolic dimension was also noted. Cardiac dysrhythmias have been documented in a few reports, due to the left ventricular remodelling that occur in this disease although no such rhythm abnormality was noted in our case [8]. Treatment was aimed at removing the source of GH hypersecretion or at suppressing its activity. Somatostatin analogues are effective as first-line therapy and have a success rate of about 50% [9]. In our case, for definitive treatment, we referred the patient to Neurosurgery Department for curative resection of the tumor, thus obliterating the source of GH hypersecretion.
References
- Colao A, Ferone D, Marzullo P, Lombardi G. Systemic complications of acromegaly: epidemiology, pathogenesis, and management. Endocr Rev 2004;25(1):102-152.
- Sacca L, Cittadini A, Fazio F. Growth hormone and the heart. Endocr Rev 1994;15:555-573.
- Corville C, Mason WR. The heart in acromegaly. Arch Int Med 1998;61:704-713.
- Colao A, Marzullo PD, Somma C, Lombardi G. Growth hormone and the heart. Clin Endocrinol (Oxf) 2001;54:137-154.
- Bertoni PD, Morandi G. Impaired left ventricular diastolic function in acromegaly: an echocardiographic study. Acta Cardiol 1998;42:1-10.
- Rodrigues EA, Caruana MP, Lahiri A, Nabarro JDN, Jacobs HS, Raftery EB. Subclinical cardiac dysfunction in acromegaly: evidence for a specific disease of heart muscle. British Heart J 1989;62:185-194.
- Damjanovic SS, Neskovic AN, Petakov MS, Popovic V, Vujisic B, Petrovic M, et al. High output heart failure in patients with newly diagnosed acromegaly. Am J Med 2002;112:610-616.
- Kahaly G, Olshausen KV, Mohr–Kahaly S, Erbel R, Boor S, Beyer J, et al. Arrythmia profile in acromegaly. Eur Heart J 1992;13(1):51-56.
- Hayward RP, Emanuel RW, Nabarro JDN. Acromegalic heart disease: influence of treatment of acromegaly on the heart. Q J Med 1987;62:41-58.
|