Introduction
Ovarian germ cell tumors (GCTs) are derived from primordial germ cells of the ovary. They may be benign or malignant and comprise about 30% of ovarian neoplasms and 3% of all malignant ovarian neoplasms. They arise in young women between 10 and 30 years of age [1]. These tumors grow rapidly, and present with a large ovarian mass with early stage disease. Malignant GCTs are classified into subgroups, the most common of which is dysgerminoma. It is the female counterpart of testicular seminoma in males [2,3]. Patients present with abdominal distention, dull pain, with raised ß-human chorionic gonadotropin (ß-hCG) levels [3].
Our case presented with marked abdominal distention, without any symptom of loss of weight, appetite or any gynecological problem. Such a presentation may be unusual for such a large malignant ovarian mass.
Case Report
The patient was a 9 year young girl who presented with abdominal distention and dull pain. There was no history of nausea and vomiting. She was non-menstruating with negative history of any prior gynecology related problem. On general abdominal examination, a huge intra-abdominal mass was palpable which was mildly mobile in nature. The lower limit was not ascertained.
The routine biochemical tests like hemoglobin, total and differential leukocyte count, urine routine and culture were within normal limits. Liver function test showed mild elevation of liver enzymes while lipase and amylase values were normal. ß-human chorionic gonadotropin (ß-hCG) levels were not done initially in the course of diagnosis as the ovarian mass was not suspected due to absence of any strong gynecological symptoms.
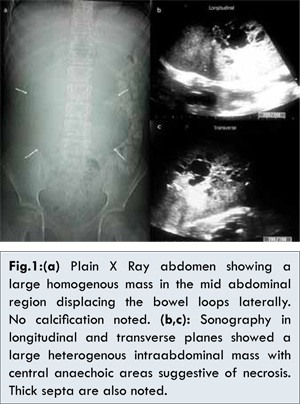
Plain X ray abdomen showed a large homogenous mass filling the mid part of the abdomen and causing displacement of bowel loops laterally. No calcification could be elicited [Fig.1a]. However, minimal fluid was seen in the pelvis. Ultrasound abdomen showed a large heterogeneous lobulated abdominal mass reaching up to the pelvic brim. It measured about 15x13.2x16.3 cm in size and showed central areas of necrosis with a few small specks of calcification [Fig.1b,c]. Minimal fluid was noted in the pelvic cavity. Since the mass was extremely large in size filling almost whole of the abdominal cavity, the origin of the mass could not be determined. Uterus was pubertal in size and was displaced by the mass towards the left side. Endometrial cavity was normal. Ovaries could not be localized on sonography. On Color Doppler study, the mass showed significant vascularity inside it with a few tortuous vessels entering into it on the right side. These vessels showed increased flow with low resistive and low impedance flow pattern.
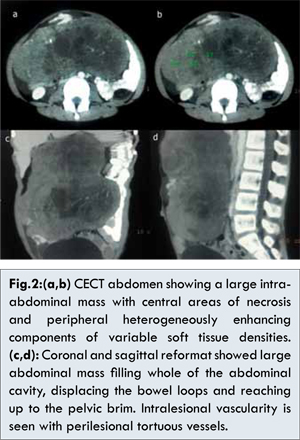
CECT abdomen was done after giving oral as well as intravenous contrast to determine the site of origin and characterization of the mass. It showed a large well defined lobulated heterogeneously enhancing mass with 59-61 HU occupying most of the mid-part of abdomen and reaching up to the pelvic brim. Multiple areas of necrosis with a few small specks of calcification were noted. Significant contrast filled vessels were seen in and around this lesion suggestive of moderately vascular in nature. Large tortuous enhancing vessels were seen entering through its anterior wall extending along its right lateral border reaching down up to the pelvic brim [Fig.2a-d]. The vessels appear to be arising from the internal iliac artery on the right side with multiple tortuous dilated vessels in the right parametrial region. The contrast filled bowel loops were displaced laterally and posteriorly by this mass. Pancreas was compressed posteriorly. Ovaries still could not be localized and origin of mass was still not determined. Uterus was displaced towards the left side. Right kidney was normal in size, shape and attenuation with moderate degree of hydronephrosis. Upper third of right ureter was dilated. No calculus was seen. Left kidney was normal in size, attenuation and enhancement. Left ureter was not dilated.
A few enlarged lymph nodes are seen along the mesentery and lower para-aortic region, the largest measuring a 19x13 mm in size. Small amount of free fluid was seen in the pelvis. Laparotomy was done under general anesthesia. Mass was well defined without any evidence of adjacent infiltration. A large well defined mass resected without any per operative complications. No adherence was noted to adjacent bowel loops. Surprising the mass was localized to the right ovary with multiple tortuous vessels arising from the pelvis and entering into this mass through a pedicle [Fig.3a,b].
Histopathological examination of the resected mass was sent to the pathology department. On gross examination, the specimen was of pinkish grey hue. The cut section showed areas of necrosis with thick septa in the center of the mass corroborating with the radiological findings of sonography and computed tomography [Fig.3c,d]. Hematoxylin-eosin stained slides under high power microscope showed monotonous population of cells resembling primordial germ cells arranged in small nests. The nests are separated by fibrous septa infiltrated by occasional small lymphocytes. The scattered multinucleate giant cells, syncitioblast were also seen [Fig.4a,b].
The final diagnosis of malignant germ cell tumor-dysgerminoma was made and at present child is undergoing chemotherapy.
Discussion
Dysgerminomas are tumors composed of cells that are similar to primordial germ cells. They display a striking similarity to their testicular counterpart, the seminoma. Dysgerminomas are solid, white or grayish white tumors. Unilateral tumors are more common in the right ovary, and 10-20% of dysgerminomas are bilateral. Most cases occur in the second and third decades of life. Dysgerminomas account for about 2% of all ovarian tumors and only 3–5% of all malignant ovarian tumors. High prevalence has been reported in Japan and India [4].
Choriocarcinomas are rare and often are admixed with other germ cell tumors. Primary ovarian choriocarcinomas occur in children and young adults. Choriocarcinomas are highly malignant and locally invasive, spread extensively throughout the abdominal cavity, and metastasize early. Nongestational choriocarcinomas spread mainly via lymphatics, whereas gestational choriocarcinomas spread primarily via the bloodstream [4].
Secretion of human chorionic gonadotropin may cause precocious puberty and may be used as a tumor marker. Analysis of ß-hCG, AFP or LDH might be helpful for making a correct diagnosis before surgery [2]. At Magnetic Resonance Imaging and computed tomography, dysgerminomas also appear as lobulated solid tumors with central areas of necrosis and small specks of calcification [5]. The characteristic features of ovarian dysgerminoma on sonography findings is a purely solid tumor divided into different lobules, with irregular internal echogenicity, with smooth lobulated contours and well defined borders, and richly vascularized at color Doppler examination [6,7].
The microscopic appearance of ovarian dysgerminoma is identical to that of testicular seminoma. They are composed of a monotonous round cells resembling primordial germ cells diffusely arrangement. The tumor cells are polygonal, with discrete cell membranes and abundant eosinophil to clear glycogen-rich cytoplasm. The nuclei are large, central and rounded, and they contain one or a few prominent nucleoli [8].
After post-surgical resection of the mass, histopathological examination, raised ß-human chorionic gonadotropin (ß-hCG) levels 158 mIU/mL, the diagnosis of malignant germ cell tumor (dysgerminoma) stage Ib was made.
Survival has improved considerably since the implementation of combination chemotherapy [9]. The child is presently undergoing chemotherapy. ß-human chorionic gonadotropin (ß-hCG) levels are gradually coming down to normal levels indicating that the disease has not progressed and is normalizing.
Conclusion
The careful surgical staging, conservative surgery for unilateral disease, followed by adjuvant chemotherapy, seems to be the ideal treatment in cases of ovarian dysgerminoma.
References
- Zalel Y, Piura B, Elchalal U, Czernobilsky B, Antebi S, Dgani R. Diagnosis and management of malignant germ cell ovarian tumors in young females. Int J Gynaecol Obstet 1996;55:1-10.
- Zaloudek C. The ovary. In: Gompel C, Silverberg SG (eds). Pathology in Gynecology and Obstetrics. Philadelphia, PA: JB Lippincott Co;1994:379-397.
- Noam Lazebnik, Anna Balog, Shirley Bennett, Raymond Redline, James Liu. Ovarian Dysgerminoma: A Challenging Clinical and Sonographic Diagnosis. J Ultrasound Med 2009;28:1409-1415.
- Kurman R. Blaustein’s pathology of the female genital tract. New York: Springer-Verlag, 1994.
- Kim HS, Kang BS. Ovarian dysgerminoma: color Doppler ultrasonographic findings and comparison with CT and MR imaging findings. J Ultrasound Med 1995;14:843-848.
- Valentin L, Ameye L, Testa A, L´ecuru F, Bernard JP, Paladini D, Van Huffel S, Timmerman D. Ultrasound characteristics of different types of adnexal malignancies. Gynecol Oncol 2006;102:41-48.
- S. Guerriero A, C Testa, D Timmerman, C Van Holsbeke, S Ajossa, D Fischerova, et al. Imaging of gynecological disease: clinical and ultrasound characteristics of ovarian dysgerminoma. Ultra Obstet Gynecol. 2011;37:596–602.
- Prat J. Germ cell tumors. In: Prat J (ed) Pathology of the Ovary. Saunders: Philadelphia, PA, 2004;251-282.
- Pectasides D, Pectasides E, Kassanos D. Germ cell tumors of the ovary. Cancer Treat Rev 2008;34:427-441.