Rajshree Dayanand Katke1, Mehul S Bhansali2, Dhruv Gohil3
From the 1Department of Obstetrics & Gynecology, Cama & Albless Hospital, Grant Government Medical College & Sir J. J. Group of Hospitals, Mumbai; Departments of 2Radiotherapy, 3Obstetrics & Gynecology, Grant Government Medical College & Sir J. J. Group of Hospitals, Mumbai, Maharashtra, India.
Corresponding Author:
Dr. Rajshree Dayanand Katke
Email: drrajshrikatke@gmail.com
Abstract
Introduction: Clear cell carcinomas of ovary are extremely rare tumors accounting for less than 5% of cases and have a very poor prognosis in terms of survival and response to chemotherapy. Case Reports: We document 3 cases of clear cell carcinoma treated by debulking surgery of ovarian mass with hysterectomy, omentectomy, bilateral pelvic lymph node dissection and chemotherapy. Discussion: Standard treatment of epithelial ovarian cancer (EOC) including clear cell carcinoma involves primary optimal debulking surgery followed by cisplatin/paclitaxel based chemotherapy. Overall 5-year survival rate remains quite low, approximately 40%, probably as a result of the lack of effective therapies.
|
6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ff6c00060000006603000001001100 6go6ckt5b5idvals|409 6go6ckt5b5|2000F757Tab_Articles|Fulltext Introduction
Ovarian clear cell adenocarcinomas (OCCAs) account for <5% of all ovarian malignancies, and 3.7–12.1% of all epithelial ovarian carcinomas (EOCs) [1-4]. They were originally described by Schiller in 1939, who coined the term “mesonephroma” to describe an ovarian neoplasm comprised of clear and hobnailed cells with an immature glomerular pattern [5,6]. In 1973, the World Health Organization (WHO) strictly defined ovarian clear cell carcinomas (OCCCs) as lesions characterized by clear cells growing in solid, tubular or grandular patterns as well as hobnail cells lining tubules and cysts. Subsequently, it was observed that Schiller’s original descriptions actually included two distinct populations: a highly malignant germ cell tumor occurring in younger women, and another tumor of epithelial origin with a less aggressive phenotype, which was formally designated as ovarian clear cell carcinoma in 1973 by the World Health Organization [5-7]. Herein we report three extremely rare cases of clear cell carcinoma of ovary with multiple medical problems who were refused treatment at many other hospitals and were treated successfully at our tertiary care centre with debulking surgery followed by chemotherapy (carboplatin + paclitaxel based).
Case Reports
Case 1
A 46 year female with history of multiple medical problems like bronchial asthma, ischemic heart disease, hypertension on treatment presented with complaints of pain in abdomen since 1 year. Pain was insidious in onset, gradually progressive, dull aching, non-radiating and associated with vomiting. She was unmarried, postmenopausal since 2 years with regular menstrual cycles in the past. On examination, her vitals were stable. On per abdomen examination, 34 weeks size firm mass arising from pelvis with restricted mobility was seen which was confirmed on per vaginal examination. Cervix, vagina were healthy on per speculum examination.
Fine needle aspiration cytology was suggestive of epithelial neoplasm. CT scan of abdomen showed 17.5x10.4x21 cm well defined solid cystic lesion seen to be arising from right adnexa in pelvis. Right ovary was not seen separately. Uterus measured 7.1x4.7x4 cm and 3.6x2.7 cm sized fibroid was seen in left lateral wall laterally compressing ureter causing hydroureter and hydronephrosis. CA 125 levels were 41.69 U/mL.
Exploratory laprotomy with debulking of ovarian mass with hysterectomy with omentectomy with bilateral pelvic lymph node dissection was done. Large ovarian, bosselated, encapsulated, vascular mass with size of 25x25x20 cm having large pedicles and adhesions with omentum and mesentry was resected [Fig.1a,1b]. Histopathology was suggestive of moderately differentiated clear cell carcinoma. Fluid showed isolated malignant cells with foci of hemorrhage. Post operatively, patient received 6 cycles of carboplatin and paclitaxel based chemotherapy.
Case 2
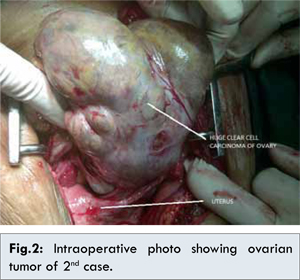
A 62 years P6L5D1 female with diabetes, hypertension & ischemic heart disease presented with complaints of abdominal pain and difficulty in defecation since 4 months. She had all full term home deliveries with tubal ligation done. She was on oral isosorbitrate, amlodipine, atorvastatin and alprazolam treatment. Her vitals were stable. Her per abdomen examination revealed ascites while her per speculum examination showed healthy cervix and vagina. Exact size of uterus could not be assessed on per vaginum examination however, pelvic tenderness was present on right side. Her CA 125 level was 123.51 U/mL, CEA - 1.24 ng/mL, AFP - 0.920 IU/mL. Pap smear was suggestive of inflammatory smear. Ascitic fluid tapping revealed of exudative ascitic fluid and suspicious cells of adenocarcinoma. CT scan was suggestive of 5x2.3 cm heterogeneously enhancing lobulated lesion noted in right adnexa and similar lesion of size 3.4x1.9 cm noted in left adnexa with moderate free fluid. Ovaries could not visualized separately from both lesions. Multiple enlarged non-necrotic lymph nodes were seen along left common iliac vessels and aorto-caval region. Multiple simple cortical cysts were seen in both kidneys along with 7 mm calculus at mid pole of left kidney. Exploratory laparotomy with de-bulking surgery and radical abdominal hysterectomy with lymph node dissection was done [Fig.2]. Frozen section report was suggestive of clear cell carcinoma. Final histopathology report revealed moderately differentiated bilateral clear cell carcinoma. Post operatively patient received 6 cycles of carboplatin and paclitaxel based chemotherapy.
Case 3
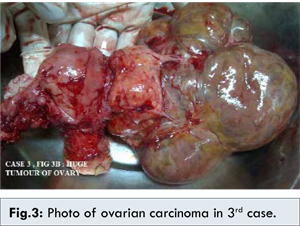
A 48 years old, P5L5, postmenopausal since 9 months, a known case of carcinoma ovary presented with abdominal pain since 15 days. She had previous history of exploratory laparotomy (details not available) and had completed 4 cycles of chemotherapy. Her past menstrual cycles were irregular and scanty. She had 5 full term home deliveries. On physical examination, she had normal vitals. Right paramedian scar of previous surgery was present on abdomen examination. Per speculum examination showed healthy cervix and vagina. On per vaginum examination 5x6 cm mass was felt in left fornix with restricted mobility. CA 125 was 130.9 U/L (0-35). CT scan report showed a lobulated enhancing predominantly cystic lesion of 5.9x5.5x5.9 cm with enhancing solid tissue within left adnexa. Both ovaries could not be separately visualized from this lesion, Enhancing sheet like omental deposits and small enhancing peritoneal deposit of size 2.5x1.6 cm were seen in pouch of Douglas. Enlarged enhancing left para-aortic nodes were seen below the level of left renal vessels, largest measuring 1.8x1.7 cm with mild free fluid. Exploratory laparotomy with total abdominal hysterectomy and left salphingo-oophorectomy with lymph node dissection with omentectomy was done [Fig.3]. Post-operatively patient received 6 cycles of carboplatin and paclitaxel based chemotherapy.
Here we are presenting three extremely rare cases of clear cell carcinoma of ovary with multiple medical problems and being refused treatment at many other hospitals which were treated successfully at our tertiary care center with debulking surgery followed by chemotherapy (carboplatin + paclitaxel based).
The current standard treatment of epithelial ovarian cancer (EOC) including clear cell carcinoma involves primary optimal debulking surgery followed by paclitaxel/carboplatin-based chemotherapy. Despite, however, the significant advances in surgery and chemotherapy achieved over the past decades, the resulting overall 5-year survival rate in patients presenting with advanced-stage disease remains quite low, approximately 40%, probably as a result of the lack of effective therapies.
Ovarian clear cell carcinoma tumors represent 5-25% of ovarian cancers. Its histologic diagnosis can be challenging, resulting often times in misclassification of these tumours. Ovarian clear cell carcinoma tends to present at earlier stages and has been associated with endometriosis, ARID1A and PIK3CA mutations. The patients with early-stage ovarian clear cell carcinoma have a better prognosis than patients with high-grade serous tumours. For patients with advanced stage disease, high-grade serous histology confers a better prognosis than ovarian clear cell carcinoma.
When compared with their serous counterparts, a greater proportion of ovarian clear cell adenocarcinomas tumors present at early-stage due to large pelvic mass, which may account for their earlier diagnosis. Histopathologically, they consist of large cuboidal, hobnailed or flattened epithelial cells containing abundant clear cytoplasm lining tubules and cysts, and growing in solid/tubular or glandular patterns. In addition, an oncocytic (oxyphilic) variant of OCCA also exists, where the tumor cells have eosinophilic rather than clear cytoplasm [8]. An increased incidence of vascular thrombotic events and hypercalcaemia is seen in patients with OCCA, with a higher frequency of lymph node metastases also being noted for these patients among the non-serous types of EOCs [9,10].
Poor prognostic factors in OCCA include young age (<60 years), advanced stage of disease and the presence of vascular invasion, whereas the presence of a predominantly (>75%) papillary or tubulocystic morphological pattern independently predicts a better prognosis [4]. With regard to the histological grading of OCCA tumors, no formal consensus exists [11,12]. Although the vast majority of OCCA tumors are considered to be of high grade, histological grading of these tumors has shown no prognostic value [13].
The general consensus from numerous retrospective studies is that, at advanced stages (stage III/IV), OCCA carries a poor prognosis with insensitivity to platinum-based chemotherapy relative to serous and other non-clear cell EOCs [4].
Conclusion
The management of ovarian cancers is difficult and requires great expertise and experience due to complications encountered while operating. Presence of an oncology department at our center helps us to a great deal in the chemotherapy management of such cases.
References
- Schiller W. Mesonephroma ovarii. Am J Cancer. 1939;35:1-21.
- Aure JC, Hoeg K, Kolstad P. Mesonephroid tumors of the ovary: clinical and histopathologic studies. Obstet Gynecol. 1971;37:860-867.
- Kennedy AW, Biscotti CV, Hart WR, Webster KD. Ovarian clear cell adenocarcinoma. Gynecol Oncol. 1989;32:342-349.
- Crozier MA, Copeland LJ, Silva EG, Gershenson DW, Stringer CA. Clear cell carcinoma of the ovary: a study of 59 cases. Gynecol Oncol. 1989;35:199-203.
- O’Brien ME, Schofield JB, Tan S, Fryatt I, Fisher C, Wiltshaw E. Clear cell epithelial ovarian cancer (mesonephroid): bad prognosis only in early stages. Gynecol Oncol.1993;49:250-254.
- Sugawa T, Umesaki N, Yajima A, Satoh S, Terashima Y, Ochiai K, et al. A group study on prognosis of ovarian cancer. Acta Obstet Gynaecol Jpn. 1992;44:827-832.
- Jenison EL, Montag AG, Griffiths CT, Welch WR, Lavin PT, Greer J, et al. Clear cell adenocarcinoma of the ovary: a clinical analysis and comparison with serous carcinoma. Gynecol Oncol. 1989;32:65-71.
- Goff BA, Sainzdela Cuesta R, Muntz HG, Fleischhacker D, Ek M, Rice LW, et al. Clear cell carcinoma of the ovary: a distinct histologic type with poor prognosis and resistance to platinum-based chemotherapy in stage III disease. Gynecol Oncol. 1996;60:412-417.
- Behbakht K, Randall TC, Benjamin I, Morgan MA, King S, Rubin SC. Clinical characteristics of clear cell carcinoma of the ovary. Gynecol Oncol. 1998;70:255-228.
- Recio FO, Piver MS, Hempling RE, Driscoll DL. Lack of improved survival plus increase in thromboembolic complications in patients with clear cell carcinoma of the ovary treated with platinum versus nonplatinum-based chemotherapy. Cancer. 1996;78:2157-2163.
- McGuire WP, Hoskins WJ, Brady MF, Kucera PR, Partridge EE, Look KY, et al. Cyclophosphamide and cisplatin compared with paclitaxel and cisplatin in patients with stage III and stage IV ovarian cancer. N Engl J Med. 1996;334:1-6.
- Creemers GJ, Bolis G, Gore M, Scarfone G, Lacave AJ, Guastalla JP, et al. Topotecan, an active drug in the second-line treatment of epithelial ovarian cancer: results of a large European phase II study. J Clin Oncol. 1996;14:3056-3061.
- Shimizu Y, Umezawa S, Utsugi K, Hasumi K, Fujiwara K, Kohno I. Combination of CPT-11 with mitomycin-C (MMC) for platinum-refractory clear cell (CCA) and mucinous (MCA) adenocarcinoma of the ovary [abstract 1393]. Proc Am Soc Clin Oncol. 1999;18:361a
|