Introduction
Testicular ischaemia is a rare consequence of inguinal hernia repairs. Ischaemic orchitis leading to testicular atrophy occurs in 0.2-1.1% of all inguinal hernia repairs [1]. It typically presents 2-3 days after the surgery and can lead to infarction [2]. This case report describes a 53 year old male who developed testicular infarction post-open inguinal hernia repair. The risk factors for developing testicular ischaemia and whether the type of hernia repair approach (open versus laparoscopic) has effects on testicular perfusion postoperatively will also be discussed.
Case Report
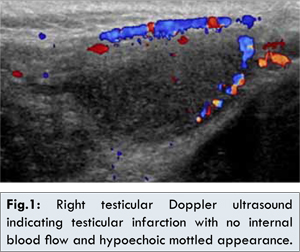
52 year old male, Mr A, presented with a recurrent large right inguinal hernia (IH). His past history includes a right vasectomy and open repair of a right IH done 2 years ago with no mesh inserted. He underwent an open tension-free repair of the inguinal hernia with prolene mesh. The procedure was technically difficult and required more diathermy use and increased spermatic cord dissection due to the large hernia and previous surgery causing fibrosis. He was discharged the next day with no obvious complications. He represented 2 days later with fevers, right iliac fossa pain and right scrotal pain and swelling. His white cell count was elevated at 14.5 (4-11x109/L), haemoglobin 17 (14-18 gm/dL) and CRP 203 (<3). He was prescribed intravenous ceftriaxone to treat for an infective cause. He had a urine culture, blood cultures and a wound swab done as well. He underwent a testicular ultrasound which showed an oedematous right scrotal wall. The right testis showed no internal blood flow on Doppler interrogation and had a hypoechoic mottled appearance. These features were consistent with testicular infarction [Fig.1]. After discussion with the patient himself, it was decided he would be treated conservatively. He was discharged when his symptoms abated 2 days later and cultures taken were all negative.
The vascular supply of the testes is mostly from the testicular arteries derived from the abdominal aorta. Collateral arterial supply exists from the cremasteric artery and artery to the vas deferens. Venous drainage is via the pampiniform plexus to the testicular veins [1].
Testicular ischaemia is mostly caused by spermatic cord torsion. Other rarer causes include inguinal hernia repairs and severe epididymitis [1,3,4]. As with Mr A, patients usually experience pain and swelling which may become asymptomatic later [2]. Commonly, orchitis is caused by damage to the pampiniform plexus which leads to venous congestion and acute thrombosis [2]. This is more common than inappropriate closure of the inguinal canal or arterial compromise due to the presence of collateral blood supply [2].
Factors increasing the risk of ischaemic orchitis include recurrent hernia repairs, large indirect hernias, previous/concomitant scrotal surgery including vasectomies which may disrupt collateral blood supply of the testes and diathermy usage [2]. It typically presents 2-3 days after the surgery and can lead to infarction [2]. This was the case with Mr A, who presented only 2 days after the hernia repair with scrotal pain and swelling.
The incidence of ischaemic orchitis after open repairs is 0.6% [5]. Orchitis is thought to be more common after open approaches associated with large indirect and recurrent inguinal hernias due to greater manipulation of the spermatic cord beyond the pubic tubercle and during dissection of the distal hernial sac [2]. Mr A also had a large recurrent hernia requiring difficult dissection of the sac distally and this together with increased diathermy usage could have resulted in pampiniform plexus damage leading to testicular ischemia. The incidence after laparoscopic repairs is 0.08% due to reduced spermatic cord dissection. This was seen in a prospective cohort study of 976 patients over 6 years who underwent a laparoscopic totally extraperitoneal approache (TEP). Follow up on patients ranged from 6 to 79 months [6]. The incidence is 5% in recurrent cases [6].
A prospective cohort study of 37 men aged 18 to 70 years old was done over a 1 year period to study the effects of open (17 patients) and laparoscopic herniorraphy (TEP 20 patients) on testicular function. Subjects underwent Doppler ultrasonography and serum testicular hormone analysis pre and post open repair or TEP. Testicular function was measured up to 6 months post repair. Preoperatively, there was significant elevation in the sonographic resistive index (RI) in the affected side (mean 0.601 vs 0.569, p<0.001). Resistive index was measured as (systolic peak velocity- end diastolic peak velocity)/ systolic peak velocity. There were significant reductions in RI for both laparoscopic (p=0.016) and open methods (p<0.001), however there was no significant difference between these reductions in RI (p=0.34). The study also found that there was no change in testicular volume and hormonal values including FSH/LH, testosterone levels pre and post operatively. Open and laparoscopic repair did not alter outcomes of testicular function up till 6 months and there were improvements in testicular perfusion for both [7].
A metanalysis done between January 1992 and March 2013 consisting of 1157 patients explored testicular complications after open and TEP approaches. However, there were no differences in testicular problems including ischaemia (p=0.453), operative time, hernia recurrence, chronic pain, seromas/haematomas and wound infections [8].
A randomized controlled trial of 120 patients done to study testicular function after laparoscopic (60 patients) and open (57 patients) mesh repair of inguinal hernias favoured the laparoscopic approach. The laparoscopic group consisted of transabdominal preperitoneal (TAPP) (28 patients) and TEP (32 patients) approaches. Testicular function was measured by testicular volume, blood flow and hormones pre operatively and 3 months post-operatively. There was a decrease in resistive index for both groups but it was significant after a laparoscopic repair (0.64 vs 0.58, p=0.04) and not after an open one (0.68 vs 0.65, p=0.07). There was a decrease in testicular volume (cm3) for both (open 10.7 vs 9.2 and lap 9.8 vs 9.3) but this was significant in the open group (p=0.01). There was a significant decrease in serum testosterone levels only in the open group again (p=0.02) [9].
A case series done in the UK between 1982 and 1991, consisted of 9 patients between the ages of 19 and 68 who had undergone open inguinal hernia repairs and had presented subsequently with testicular ischaemia. 7 had history of previous repairs or complicated surgeries. The study found that patients with recurrent hernias, previous scrotal surgeries and possibly vasectomy are at increased risk of developing testicular ischaemia [10]. Mr A also previously had had a vasectomy and large IH repair on the affected side resulting in a complicated repeat repair. Nyphus 1988 found that less testicular atrophy is possible if the cord is mobilized more proximally as there is less trauma to the blood supply and pampiniform plexus [11].
Conclusion
The risk of testicular ischaemia is increased in those with large or recurrent hernias and difficult open repairs such as in Mr A. Thus, male patients undergoing IH repairs should be informed about this rare complication.
Acknowledgements
We would like to thank the General Surgery Department at Werribee Mercy Hospital for undertaking care of this patient.
References
- Dellabianca C, Bonardi M, Alessi S. Testicular ischaemia after inguinal hernia repair. J Ultrasound. 2011;14(4):205-207.
- Moore JB, Hasenboehler EA. Orchiectomy as a result of ischaemic orchitis after laparoscopic inguinal hernia repair: case report of a rare complication. Patient Saf Surg. 2007;1:3.
- Meier AH, Ricketts RR. Surgical complications of inguinal and abdominal wall hernias. Semin Pediatr Surg. 2003;12:83-88.
- Ridgway PF, Shah J, Darzi AW. Male genital tract injuries after comtemporary inguinal hernia repair. BJU Int. 2002;90:272-276.
- Wantz GE. Complications of inguinal hernial repair. Surg Clin North Am. 1984;64:287-298.
- Vanclooster P, Smet B, de Gheldere C, Segers K. Laparoscopic inguinal hernia repair: review of 6 years experience. Acta Chir Belg. 2001;101:135-138.
- Beddy P, Ridgway PF, Geoghegan T, Pierce C, Govender P, Keane FB, et al. Inguinal Hernia Repair Protects Testicular Function: A Prospective Study of Open vs Laparoscopic Herniorraphy. J Am Coll Surg. 2006;203:17-23.
- Zhu X, Cao H, Ma Y, Yuan A, et al. Total extraperitoneal laparoscopic hernioplasty versus open extraperitoneal approach for inguinal hernia repair: A meta- analysis of outcomes. The Surgeon. 2014;12:94-105.
- Singh AN, Bansal VK, Misra MC, Kumar S, Rajeshwari S, Kumar A, et al. Testicular functions, chronic groin pain, and quality of life after laparoscopic and open mesh repair of inguinal hernia: a prospective randomised controlled trial. Surg Endsoc. 2012;26:1304-1317.
- Reid I, Devlin HB. Testicular atrophy as a consequence of inguinal hernia repair. British Journal of Surgery. 1994;81:91-93.
- Nyhus LM, Pollak R, Bombeck CT, Donahue PE. The preperitoneal approach and prosthetic buttress repair for recurrent hernia. The evolution of a technique. Ann Surg. 1988;208:733-737.