Introduction
Meckel’s diverticulum has been described as the remnant of the omphalo-mesenteric duct and is the most common congenital abnormality of the gastrointestinal tract. It is present in about 2% of the population at a ratio of 3 males to 1 female. It has length 10-12 cm and is situated in a distance of 30-60 cm from the ileocaecal valve. Meckel’s diverticulum may contain intestinal mucosa or heterotopic gastric or pancreatic tissue.
Most patients are asymptomatic but patients with clinical symptoms have a higher incidence of heterotopic tissue [1,2]. When patients with a Meckel’s diverticulum develop symptoms; a complication is almost always present. The principal complications of Meckel’s diverticulum include ulceration, hemorrhage, small bowel obstruction, diverticulitis, and perforation [3].
Case Report
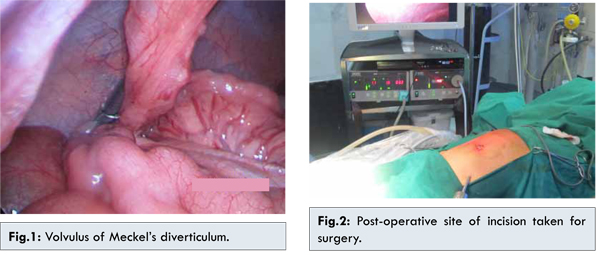
A 5 year old child was admitted in emergency with history of generalized abdominal pain followed by bilious vomiting of one day duration. There was no history of any fever, loose motions, or any urinary symptoms. His past medical history was suggestive of similar signs and symptoms at the age of 2½ years. In that admission his X-ray abdomen had shown few air fluid levels and ultrasound abdomen was within normal limits. He was managed conservatively. He remained asymptomatic till the present admission. His first clinical examination revealed body temperature of 99oF, heart rate of 105 beats/minute and respiratory rate of 24/min with moderate dehydration. An examination of abdomen showed abdominal distension with generalized tenderness, more in central abdomen. No rebound tenderness or guarding was noted. On investigating, X-ray abdomen showed few dilated loops of small bowel on left side of abdomen with normal large bowel. There was no evidence of gas under diaphragm. Ultrasound abdomen was suggestive of small bowel intussusceptions. A C.T. scan abdomen showed presence of long Meckel’s diverticulum attached to umbilicus, with its volvulus along the axis leading to small bowel obstruction. The Meckel’s diverticulum was attached to umbilicus with a twist at it’s base. Bowel loops proximal to diverticulum were dilated. The child was posted for laparoscopic surgery after correcting imbalance of electrolytes. Abdomen was entered after creating pneumo-peritoneum with Veress needle. A 5 mm port was placed in left hypochondriac region and initial diagnostic laparoscopy carried out. At laparoscopy findings of C.T. scan were confirmed (Fig.1 showing laparoscopic view of twisted Meckel’s diverticulum). Laparoscopy showed long twisted Meckel’s diverticulum arising from ileum attached to abdominal wall at umbilicus with dilated proximal small bowel loops and small amount of free fluid in peritoneal cavity. The attachment of Meckel’s diverticulum to umbilicus was divided with bipolar cautery. The Meckel’s diverticulum was blind ending at umbilicus. There was no evidence of communication of diverticula with umbilicus suggesting patent omphalomesentric duct. Then through small semicircular incision of 3 cm around umbilicus, diverticulum was delivered outside. It was divided with linear stapler. Post-operative recovery was uneventful (Fig.2 showing small semicircular incision taken to deliver Meckel’s diverticulum).
Most Meckel’s diverticula are asymptomatic and are found either during autopsy or incidentally on laparotomy, laparoscopy, or barium study for other abdominal conditions. It is controversial whether to attempt surgical correction of an asymptomatic Meckel’s diverticulum found incidentally as the risk of developing postoperative complications may be as high as 8% in such cases When patients with a Meckel’s diverticulum develop symptoms, a complication is almost always present. The principal complications of Meckel’s diverticulum include ulceration, hemorrhage, small bowel obstruction, diverticulitis, and perforation. The Meckel’s rule of 2’s is that it occurs in 2% of the population, 2% of those with a Meckel’s diverticulum will manifest clinical problems, located 2 feet proximal to the ileocecal valve and the diverticulum is approximately 2 inches long, and symptoms commonly manifest at age of 2 years [2].
Ulceration with subsequent hemorrhage (often hemodynamically significant, but usually not life threatening) is the most common complication, with an incidence of about 20-30% of all complications. It is more common in children younger than 2 years and in males. The most common presentation is painless hematochezia [4]. Intestinal obstruction is second frequent complication and is observed in 20-25% of all symptomatic Meckel’s diverticula and is attributable to intussusception, volvulus (often twisting around a persisting umbilical remnant), herniation, or entrapment of a loop of bowel through a defect in the diverticular mesentery [5]. Patients with intestinal obstruction due to Meckel’s diverticulum are usually older and present with abdominal pain, and vomiting [6].
Here we present a rare case in which volvulus developed due to twisting around a persisting umbilical remnant. A literature review of online publication showed two case reports of volvulus of Meckel’s diverticulum in children [2,7,8]. Intussusception of Meckel’s diverticulum leading to intestinal obstruction is common but very few cases of volvulus of Meckel’s diverticulum have been documented. Secondly we did laparoscopy assisted surgery. After confirming the diagnosis and dividing attachment of diverticulum to umbilicus, instead of horizontal or vertical incision, we took semi-circular incision around umbilicus to deliver Meckel’s diverticulum and divide it. This approach concealed the scar of surgery and laparoscopy helped to avoid big incision.
Conclusion
In children, Meckel’s diverticulum should be considered in differential diagnosis of acute abdomen. In a child having acute intestinal obstruction, complications of Meckel’s diverticulum should be suspected. Meckel’s diverticulum can be managed laparoscopically (or laparoscopy assisted) to give better result and faster recovery to patient.
References
- Loannis S, Vassilios L, Christopher E. An unusual case of intestinal obstruction by volvulus of Meckel’s diverticulum in a 10-year-old child: a case report. Aristotle University Medical Journal. 2014;41(2):27-29.
- Shah MY, Sonarkar R, Sahu D, Gedam BS.Large Enterolith in a Perforated Meckel’s Diverticulum: A Rare Cause of Acute Abdomen. Journal of Case Reports. 2012;2(2):89-91
- Kuwajerwala NK, Silva YJ. Meckel Diverticulum. In: Daily BJ, Talavera F, Friedman AL, Zamboni P, Geibel J (eds). eMedicine Journal:2002;3(7).
- Crawford JM. The Gastrointestinal Tract. In: Cotran RS, Kumar V, Collins T (eds). Robbins Pathologic Basis of Disease, 6th edition. 1999, Philadelphia: W. B. Saunders Company, pp. 804-805.
- Matsagas MI, Fatouros M, Koulouras B. Incidence, complications, and management of Meckel’s diverticulum. Arch Surg. 1995;130(2):143-146.
- Yamamoto LG. Bowel Obstruction With Intra-Intestinal Sand. In: Radiology Cases In Pediatric Emergency Medicine, 1996, Volume 5, Case 19.
- Charokar K, Garg N. Meckel’s Diverticulum in Adults: A Preoperative Diagnostic Dilemma. Journal of Case Reports. 2014;4(2):240-244.
- Osborne MP, Hamilton G. Shailey M. Axial volvulus of Meckel’s diverticulum. Postgrad Med J. 1978;54:692-693.