Introduction
Pretibial myxedema, also known as localized myxedema, is an infiltrative dermopathy which presents as localized lesions on the skin mostly confined to the pretibial area. It most often presents as asymptomatic, bilateral, skin colored or yellowish brown, diffuse non-pitting edema in the pretibial area with waxy induration of skin. The four main clinical variants of pretibial myxedema include non-pitting edema, plaques, nodules and elephantiasis. It is nearly always associated with Graves’ disease. Pretibial myxedema results from deposition of mucin in the reticular dermis. Fibroblasts are stimulated to produce abnormally high amounts of glycosaminoglycans due to exposure to thyroid hormones. It is seen approximately in 4% of patients with Graves’ thyrotoxicosis and usually follows ophthalmopathy. Apart from treatment of the primary thyroid abnormality, topical or intralesional steroids remain the mainstay of treatment.
Case Report
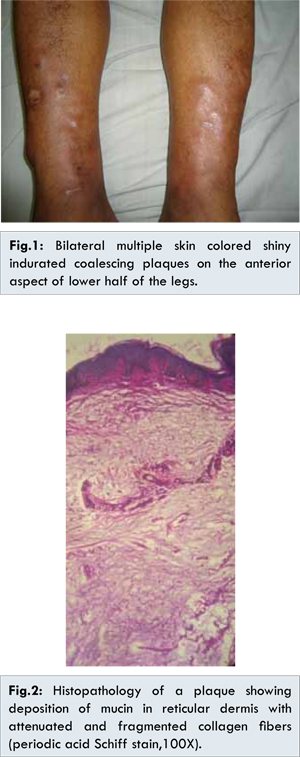
A 64 year-old man presented with asymptomatic raised skin lesions on both legs of 4 years duration. The lesions had an insidious onset with gradual progression. There was no history of trauma prior to the onset of the lesions. He was on treatment for diabetes with oral hypoglycemic agents which was well controlled. He was hypertensive also and on beta-blocker. There was no history of lethargy, cold intolerance, hoarseness of voice or constipation. On clinical examination, his vital signs were normal. His body mass index was 26.3. He had clubbing of fingers and toes. He had no pallor or lymphadenopathy. His deep tendon reflexes were delayed. There was no thyroid enlargement or exophthalmos clinically. Local examination showed bilateral symmetrical, non-tender, multiple skin colored shiny indurated coalescing plaques with loss of hair on the anterior aspect of lower half of the legs [Fig.1]. Complete blood counts, ESR, renal function tests, liver function tests, chest X-ray, serum lipid profile, fasting and postprandial blood glucose levels were within normal limits. His TSH was elevated 60 µIU /mL (normal 0.2-5 µIU/mL). Free T4 level was 0.3 ng/dL (normal 0.8-2 ng/dL) and free T3 level was 1.10 pg/mL (normal 1.4-4.4 pg/mL). Anti-thyroid antibodies were within normal limits. Differential diagnoses considered were pretibial myxedema, lichen myxedematosus and chronic obesity lymphoedematous mucinosis. Histopathology of the skin biopsy from the plaque on pretibial area showed dermal mucin accumulation with attenuated collagen fibers consistent with myxedema [Fig.2]. Thus we arrived at final diagnosis of pretibial myxedema in primary idiopathic hypothyroidism. We lost the patient for follow-up.
Pretibial myxedema (PTM) is an infiltrative dermopathy, also known localized myxedema or thyroid dermopathy. It is a rare clinical finding seen approximately in 4% of patients with Graves’ thyrotoxicosis [
1,
2]. Rarely it has been described in autoimmune thyroid diseases like Hashimoto’s thyroiditis and euthyroidism [
1,
2]. PTM can also occur after a patient has undergone radioactive iodine treatment, thyroid surgery or medical treatment for hyperthyroidism which results in a hypothyroid or euthyroid state [
3]. PTM presents as localized lesions on the skin resulting from the deposition of hyaluronic acid usually as a component of thyroid disease.
Female to male ratio is 3.5:1 [
2]. Peak age of onset is in the 5th and 6th decades. PTM most commonly presents as asymptomatic, bilateral, skin colored or yellowish brown, diffuse non pitting edema with waxy induration of skin [
4]. Four main clinical variants of PTM include non-pitting edema (43%), plaque (27%), nodular (18%) and elephantiasis (5%) [
2]. Peau d’orange appearance with prominent hair follicles, overlying hyperhidrosis or hypertrichosis, verruciform or fungating lesions may also be present. Though PTM is most commonly seen on the lateral and anterior aspects of legs, it may also present on dorsum of feet, thighs, shoulder, hands, forehead, ears or areas of trauma. PTM is primarily of a cosmetic concern. Severe elephantiasic form may lead to limb enlargement and impair function.
PTM usually starts 1-2 years after the diagnosis of Graves’ disease. Onset of dermopathy typically follows the onset of ophthalmopathy in 6-12 months. Acropachy follows dermopathy. The classical triad of ophthalmopathy, PTM and thyroid acropachy occurs in less than 1% of patients with Graves’ disease [
1].
Fibroblasts are stimulated to produce abnormally high amounts of glycosaminoglycans due to exposure to thyroid hormones. Thyrotropin and thyrotropic receptor antibodies binding sites are found in the plasma membranes of the fibroblasts from the skin of the patients with PTM. Thyrotropin receptor antibody (TRAb) is an immunoglobulin (IgG) antibody present in the serum of patients with PTM. TRAb has been demonstrated to represent thyrotropic receptor autoantibodies [
5]. TRAb is increased in 50% of patients with PTM.
A research published in 2006 shows that the change in the percentage of constituents of glycosaminoglycans lead to the development of PTM [
6]. Thyroid hormones by means of their influence on prostaglandin metabolism alter the synthesis and degradation of glycosaminoglycans. Trauma contributes to local fibroblast activation and hence PTM more in areas of injury. Fibroblasts in orbits and skin show phenotypic differences from fibroblasts in other parts of the body and this may account for the development of thyroid ophthalmopathy and dermopathy.
Histopathology shows deposition of mucin (glycosaminoglycan) in reticular dermis with attenuation of collagen fibers which are fragmented or widely separated. Stellate fibroblasts may be seen. Mucin stains blue with alcian blue at pH 2.5 and colloidal iron stains. Metachromasia is seen with toluidine blue stain.
Generalised myxedema is one of the several cutaneous changes in hypothyroidism. Generalised and pretibial myxedema have been grouped as dysthyroidotic mucinosis in a review of cutaneous mucinosis by Rongioletti and Rebora [
7]. In our case, PTM has developed in a patient with primary idiopathic hypothyroidism. In generalized myxedema which occurs in hypothyroidism, glycosaminoglycans are deposited in the skin due to impaired degradation rather than increased synthesis. We assume a similar mechanism happening locally in the pretibial area in our case of pretibial myxedema occurring in primary idiopathic hypothyroidism which is rarely reported. Salvi et al. studied 76 patients with autoimmune thyroid disease, made an echographic diagnosis of PTM in 25 (33%) patients and believe that measurement of pretibial thickness by ultrasound may be useful for revealing the presence of PTM [
8].
Pretibial myxedema like lesions may occur in chronic stasis dermatitis, but histopathology of such lesions show mucin deposition in papillary dermis along with hemosiderin deposition and nodular angiogenesis. Pretibial myxedema in euthyroid individuals is very rare and must be distinguished from chronic obesity lymphoedematous mucinosis which arises on the calves and shins of the obese [
9]. Lichen myxedematosus and focal mucinosis show histopathological findings of mucin deposition in upper dermis and proliferation of fibroblasts.
Apart from treating the thyroid abnormality, the mainstay of treatment for PTM includes local application of corticosteroids (preferably under occlusion) and intralesional injection of steroids. Wraps or stockings that provides 20-40 mmHg of pressure may be considered as an adjunctive therapy. Other treatments include octreotide injections and intravenous immunoglobulins. Intralesional injection of octreotide, a somatostatin analogue, is said to decrease dermal hyaluronic acid deposition [10]. Plasmapheresis, pentoxifylline, cytotoxic drugs and systemic steroids have shown variable results. Surgical removal is not advised as it worsens the dermopathy.
To conclude, PTM itself is a rare clinical entity. PTM in a hypothyroid patient is even rarer and may be considered as a paradox. Moreover, plaque type of pretibial myxedema is uncommon. PTM presenting as plaques in a patient with primary idiopathic hypothyroidism, as in our case, has not been reported so far.
References
- Anderson CK, Miller OF. Triad of exophthalmos, pretibial myxedema and acropachy in a patient with Graves’ disease. J Am Acad Dermatol. 2003;48(6):970-972.
- Fatourechi V. Pretibial myxedema: pathophysiology and treatment options.Am J Clin Dermatol. 2005;6(5):295-309.
- Verma S, Rongioletti F, Braun-Falco, Ruzicka T. Preradial myxedema in a euthyroid male: A distinct rarity. Dermatol Online J. 201315;19(4):9.
- Dharmalingam M, Seema G, Khaitan B, Karak A, Ammini AC. Plaque form of pretibial myxedema in hypothyroidism .Indian J Dermatol Venerol Leprol. 2001;67(6):330-331.
- Kamath C, Young S, Kabelis K, Sanders J, Adlam MA, Furmaniak J, et al. Thyrotropin receptor antibody characteristics in a woman with long standing Hashimoto’s who developed Graves’ disease and pretibial myxedema. Clin Endocrinol (Oxf). 2013;77(3):465-470.
- Komosinska-Vassev K, Winsz-Szczotka K, Olczyk K, Kozma EM. Alterations in serum glycosaminoglycan profiles in Graves’ patients. Clin Chem Lab Med. 2006;44(5):582-588.
- Rongioletti F, Rebora A. Cutaneous mucinoses: Microscopic criteria for diagnosis. Am J Dermatopathol. 2001;23(3):257-267.
- Salvi M, De Chiara F, Gardini E, Minelli R, Bianconi L, Alinovi A, Ricci R, et al. Echographic diagnosis of pretibial myxedema in patients with autoimmune thyroid disease. Eur J Endocrinol. 1994;131(2):113-119.
- Tokuda Y, Kawachi S, Marata H, Saida T. Chronic obesity lymphoedematous mucinosis: three cases of pretibial mucinosis in obese patients with pitting edema. Br J Dermatol. 2006;154(1):157-161.
- Priestley GC, Aldridge RD, Sine J, Wilson D. Skin fibroblast activity in pretibial myxedema and the effect of octreotide (Sandostatin) in vitro. Br J Dermatol. 1994;131(1):52-56.