Introduction
Squamous cell carcinoma accounts for a small proportion of bladder cancers. It has even more rarely been reported arising from the suprapubic cystostomy tract. We present a case of a 68 year old male patient who presented with squamous cell carcinoma of the suprapubic tract along with involvement of the urinary bladder. His initial suprapubic cystostomy was placed 20 years ago. The patient received palliative radiotherapy but died after four months of the diagnosis.
Case Report
A 68 year old male patient presented to us with the chief complains of a spontaneous urinary fistula from a previously healed suprapubic cystostomy (SPC) site. The fistula had been present for the past two months. His past history was significant for an open suprapubic transvesical prostatectomy performed twenty years ago. After the operation he developed recurrent episodes of obstructive LUTS and urinary retention for which he underwent multiple urethral dilations and suprapubic cytostomies. He also underwent multiple episodes of catheterization with the help of antegrade and retrograde bougie via the suprapubic tract (known as “rail roading” [
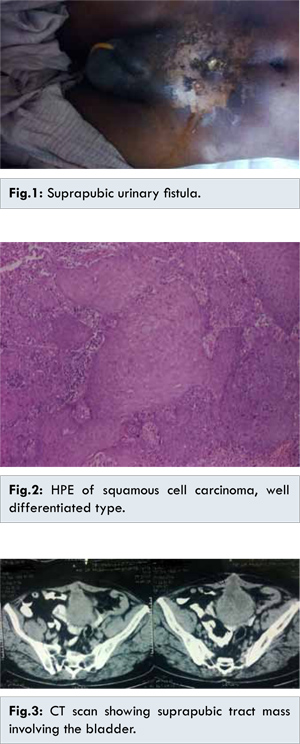
1]: The analogy of pulling one railway compartment attached to another with goods is similar to one bougie guiding the other attached to the catheter). His last urethral intervention had occurred two years ago and he was relatively symptom free since then. He was a non-smoker and had no history of overseas travel. Physical examination revealed a suprapubic urinary fistula surrounded by extensive erythematous discoloured skin [Fig.1]. A Foley’s catheter was placed per urethra without any difficulty. A biopsy taken from the edge of the fistula revealed well differentiated squamous cell carcinoma [Fig.2]. A CT scan of the abdomen revealed a mass in bladder involving the dome of the bladder and the suprapubic tract [Fig.3]. A cystoscopic biopsy of the bladder mass revealed the same histopathology. The treatment options were discussed with the patient and he chose radiotherapy refusing extensive surgery. He was treated with thirty fractions of radiotherapy with a palliative intent. The patient died after four months due to progressive disease.
Squamous cell carcinoma of the bladder occurs in about 5% of bladder carcinoma cases [
2]. It is more common in patients susceptible to chronic inflammation of bladder such as indwelling catheters and calculi, infections such as Schistosoma haematobium, or bladder diverticulum. Spinal cord injury patients have a high incidence of squamous metaplasia and bladder carcinoma due to indwelling catheters, postulated to be a result of inducible nitric oxide synthase [
3] and a incidence about 20%. About 10% cases of indwelling catheter drainage patients go on to develop squamous cell carcinoma of the bladder if left for more than 10 years [
4].
Suprapubic tract squamous cell carcinoma has been very sparsely described in literature, mostly as case reports. All cases have arisen in a background of suprapubic catheterization leading credence to the theory of chronic inflammation. Strombakis et al. is credited with the first reported case in an 80 year old patient who presented five years after SPC [
3]. Several other case reports subsequently appeared in the English literature (about ten). The age of presentation varies range 40 to 80 years [
4-
7].
The cases appear after a variable latent period of 5 to 25 years. Our patient developed the clinical picture of suprapubic fistula 20 years after the first SPC. Generally the latency in young age group being more 20-25 years [
6,
8] and in old age being short 5 to 10 years [
4,
5,
10], probably due to decreased immune surveillance and accumulating mutations with advancing age, mandating a strict surveillance protocol in old age people with SPC. The bladder may [
6,
8,
9] or may not [
4,
5,
10] be involved concomitantly. If the bladder is involved, cases may present with hematuria or positive urine cytology on cystoscopy. How the bladder involvement, affects prognosis or may impact treatment is not known because of the rarity of disease. In this case hematuria was conspicuously absent even though bladder was involved. The clinical presentation is that of a fungating skin ulcer or a spontaneous opening of a previously closed fistula with or without hematuria. In cases with concomitant bladder tumor the later presentation is more common [
6,
8,
9] while if there is no bladder involvement the malignancy presents as a new or rapidly developing ulcer [
4,
5,
10].
The treatment regimens have not been standardised, cases have been given individualised treatments usually excision alone or radiation alone or a combination of both. The amount of excision has ranged from local excision of bladder [
4,
5] to radical cystectomy [
6]. Radiation has been tried as an adjuvant, usually without making an impact. Concomitant bladder involvement mandates some sort of bladder control with diversion if patient’s general condition permit given the more aggressive nature compared to transitional cell cancer of bladder [
2].
Radiotherapy has also been tried alone [
9] generally with palliative intent as in this case. Survival has been dismal with most deaths in subsequent six to eight months irrespective of treatment modality chosen [
6,
7,
9]. As this carcinoma is rarely reported and is associated with a uniformly poor prognosis, physicians should pay immediate attention to any erythema, inflammation or mass that develops around an SPC tract and regular check cystoscopies. Radical cystectomy and urinary diversion with or without radiation appears to be the only acceptable therapy [
4-
6].
Conclusion
Squamous cell carcinoma of the suprapubic tract with or without involvement of the urinary bladder has a uniformly poor prognosis. Physicians must pay close attention to the physical examination of the suprapubic tract not only at the time of catheter change but even after catheter removal. Regular endoscopic monitoring of the urinary tract of patients on indwelling catheters must be advocated. Aggressive surgical therapy with or without radiation therapy has been described but further long term studies on the subject are required.
References
- Fowler JW, Watson G, Smith MF, MacFarlane JR. Diagnosis and Treatment of Posterior Urethral Injury. 1986;58(2-4):167-173.
- Rous SN. Squamous cell carcinoma of the bladder. J Urol. 1978;120:561-562.
- Wall BM, Dmochowski RR, Malecha M, Mangold T, Bobal MA, Cooke CR. Inducible nitric oxide synthase in the bladder of spinal cord injured patients with a chronic indwelling urinary catheter. Journal of Urology. 2001;165(5):1457-1461.
- Stroumbakis N, Choudhury MS, Hernandez-Graulau JM. Squamous cell carcinoma arising from suprapubic cystotomy site without bladder involvement. Urology. 1993;41:568-570.
- Schaafsma RJ, Delaere KP, Theunissen PH. Squamous cell carcinoma of suprapubic cystostomy tract without bladder involvement. Spinal Cord. 1999;37:373-374.
- Stokes S 3rd, Wheeler JS Jr, Reyes CV. Squamous cell carcinoma arising from a suprapubic cystostomy tract with extension into the bladder. J Urol. 1995;154:1132-1133.
- Hiroki I, Masayuki A, Hanako I, Noboru O, Ayako H, Ikuo S, et al. A case of squamous cell carcinoma arising from a suprapubic cystostomy tract. BMC Urology. 2011;1.
- Gupta NP, Singh I, Nabi G, Ansari MS, Mandal S. Marjolin’s ulcer of the suprapubic cystostomy site infiltrating the urinary bladder: a rare occurrence. Urology. 2000;56(2):330.
- Chung JM, Oh JH, Kang SH, Choi S. Squamous cell carcinoma of the suprapubic cystostomy tract with bladder involvement. J Urol. 2013;54(9):638-640.
- Massaro PA, Moore J, Rahmeh T, Morse MJ Squamous cell carcinoma of the suprapubic tract: A rare presentation in patients with chronic indwelling urinary catheters. Can Urol Assoc J. 2014;8(7-8):E510-514.
- Kaufman JM, Fam B, Jacobs SC, Gabilondo F, Yalla S, Kane JP, et al. Bladder cancer and squamous metaplasia in spinal cord injury patients. J Urol. 1977;118:967-971.