Introduction
Endometriosis was first described by Rokitansky in 1860 and was defined as the presence and proliferation of the endometrium outside the uterine cavity [
1]. It generally occurs in the pelvic sites such as ovaries, posterior cul-de-sac, uterine ligaments, pelvic peritoneum, bowel, and rectovaginal septum. Extrapelvic endometriosis is quite unusual and can be found inthe nervous system, thorax, urinary tract, gastrointestinal tract, or cutaneous tissues [
2]. Endometriosis involving the abdominal wall is a rare phenomenon. It is easily confused with other conditions, such as keloids, haematoma, stitch granuloma, abscess, inguinal and incisional hernia [
3]. The usual clinical presentation is a painful nodule in a parous woman with a history of gynecological or obstetrical surgery. The intensity of pain and size of nodule vary with menstrual cycle [
1]. Ours is a classical presentation of scar endometriosis after lower segment caesarean section.
Case Report
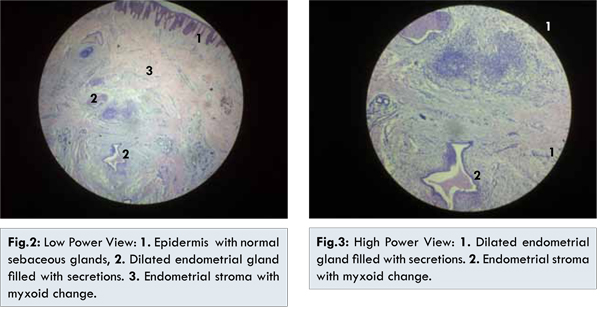
A 27 year old woman came to Gynaecology out-patient department with complaints of a painful swelling on the lower abdominal wall. She had undergone lower segment caesarean section 4 years back. Around 2 years after the surgery, she noticed a small peanut sized swelling over her scar which had gradually increased in size over the last 2 years. She also complained of pain and fullness in the swelling, especially during menses. Examination revealed a lump of around 3x3 cm at the centre of the caesarean scar, dark brown in colour, firm, tender and not fixed to the rectus sheath. Ultrasound showed a well-defined hypo-echoic lesion in the subcutaneous region just below the external scar, with no connection with the underlying muscles. Mild vascularity was noted on colour Doppler. Wide local excision of the lesion was done under local anaesthesia, which was confined to the skin and subcutaneous tissue, with no involvement of the rectus sheath. Cut section showed solid grey white tissue. Histopathology of excised mass showed epidermis and dermis. Dermis showed endometrial glands. Stroma showed myxoid change, inflammatory infiltrate and congestion. So, histopathology confirmed our diagnosis of scar endometriosis.

Scar endometriosis is most commonly seen after surgical procedures on the uterus and fallopian tubes. Incidence of scar endometriosis following hysterotomy is 1.08%-2% whereas after caesarean section the incidence is 0.03%-0.4% [
4]. The reason for higher incidence after hysterotomy could be because the early decidua has more pleuripotential capabilities and can result in cellular replication producing endometriosis. Literature reports that the average time from surgery to clinical presentation may vary from 3 months to 12 years in different series. Frequency of scar endometriosis increases with increasing number of caesarean sections and laparoscopy in the previous year’s [
5].
Direct mechanical implantation seems to be the most plausible theory for explaining scar endometriosis. During caesarean section, endometrial tissue might be seeded into the wound, and under estrogen influence these cells proliferate, producing endometriomas [
6]. This theory is convincingly demonstrated by experiments in which normal menstrual effluent transplanted to the abdominal wall resulted in subcutaneous endometriosis.
In clinical practice, its occurrence has been well documented in incisions of any type where there has been possible contact with endometrial tissue, including episiotomy, hysterotomy, ectopic pregnancy, laparoscopy, tubal ligation, and caesarean section [
7]. The presence of endometrial tissue can induce metaplasia of the surrounding fascial tissue to form an endometrioma. Alternatively, endometrial cells may reach a caesarean scar via lymphatic or haematogenous routes and subsequently grow into an endometrioma by one of the mechanisms described above. This may cause rare occurrence of abdominal wall endometrioma without any surgical intervention [
8].
Scar endometriosis is rare and difficult to diagnose, often misdiagnosed as stitch granuloma, inguinal hernia, lipoma, abscess, cyst, incisional hernia, desmoid tumor, sarcoma, lymphoma, or primary and metastatic cancer, which are a simple excuse to refer the patient to the general surgeon [
7]. A high index of suspicion is recommended when a woman presents with post-operative abdominal lump. Often, the diagnosis of endometriosis is not suggested until after histology has been performed. Correct preoperative diagnosis is achieved in 20%-50% of these patients [
9]. A good surgical and gynaecological history, as well as a thorough examination with appropriate imaging techniques (ultrasound, CT or MRI) will usually lead to a correct diagnosis. The presence of cyclic pain in an incisional mass associated with a caesarean section scar is almost pathognomonic for the condition. Some authors believe that when the diagnosis is made on clinical grounds, no further studies are necessary before wide surgical excision [
10].
Ultrasonography is the best and most commonly used investigational procedure for abdominal masses, given its practicality and lower cost. The mass may appear as a hypoechoic and heterogeneous mass with messy internal echoes. On computed tomography, the endometrioma may appear as a circumscribed solid or mixed mass, enhanced by contrast, and show haemorrhages [
11]. MRI can be more helpful when the lesion is small because of its high spatial resolution, which allows better distinction of the planes between muscles and abdominal subcutaneous tissue. Infiltration of abdominal wall and subcutaneous tissues is also much better assessed by MRI [
12]. Fine-needle aspiration cytology (FNAC) was reported in some studies for confirming the diagnosis [
13]. Histopathology is the hallmark of diagnosis. It is satisfied if endometrial glands, stroma, and hemosiderin pigment are seen [
14]. Generally, diagnosis is easy with a microscopic examination of a standard hematoxylin and eosin-stained slide. Furthermore, the cytologist’s experience is most important to clarify diagnosis and to exclude malignancy [
15].
Wide local excision with at least 1 cm margin is the treatment of choice for scar endometriosis. Larger and deeper lesions upto the muscle or the fascia are more difficult to excise completely. In large lesions, complete excision of the lesion may entail a synthetic mesh placement or tissue transfer for closure after resection [
16]. Medical treatment with the use of progestogens, oral contraceptive pills, and danazol is not effective and gives only partial relief in symptoms and does not ablate the lesion. Moreover due to side effects such as amenorrhea, weight gain, hirsutism, and acne, compliance is unlikely. Recently, there have been reports of the use of the gonadotrophin agonist (Leuprolide acetate), but it has been found to provide only prompt improvement in symptoms with no change in the lesion size [
17]. In cases of continual recurrence possibility of malignancy should be kept in mind.Good technique and proper care during caesarean section may help in preventing endometriosis. To prevent the occurrence of scar endometriosis it has been suggested that at the end of surgery especially on uterus and tubes, the abdominal wall wound should be cleaned thoroughly and irrigated vigorously with high jet solution before closure [
18].The incidence of concomitant pelvic endometriosis with scar endometriosis has been reported to be from 14.3% to 26% [
19]. Ideally, all patients must be examined for concomitant pelvic endometriosis.
Conclusion
One should have high index of suspicion of scar endometriosis when a woman presents with a painful swelling in the abdominal scar with cyclical pain, especially with a history of previous gynecological or obstetrical surgery. This condition can be confused with other surgical conditions. Efforts should be made to make a preoperative diagnosis with the help of ultrasonography. Medical treatment is not helpful. Wide local excision is the treatment of choice. Patient should be followed-up for recurrence.
References
- Khalifa Al-Jabri. Endometriosis at Caesarian Section Scar. Oman Med J. 2009;24(4):294-295.
- Jubanyik KJ, Committee F. Extrapelvic endometriosis. Obstetrics and Gynecology Clinics of North America. 1997;24(2):411-440.
- Adamo V, Di Natale W, Meola C, Gilio M, Cavalli S, Ferrari L, et al. Endometriosis in an episiotomy scar: a case report. Chirurg Ital. 2004;56:735-738.
- Chatterjee SK. Scar endometriosis: A Clinicopathological study of 17 cases. Obstet Gynecol. 1980;56:81-84.
- Aydin O. Scar endometriosis-a gynaecologic pathology often presented to the general surgeon rather than the gynaecologist: report of two cases. Langenbeck’s Archives of Surgery. 2007;392(1):105-109.
- Gunes M, Kayikcioglu F, Ozturkoglu E,Haberal A. “Incisional endometriosis after cesarean section, episiotomy and other gynecologic procedures,” Journal of Obstetrics and Gynaecology Research. 2005;31(5):471-475.
- Thapa A, Kumar A, Gupta S. Abdominal Wall Endometriosis: Report Of A Case And How Much We Know About It? The Internet Journal of Surgery. 2006;9(2).
- Bumpers HL, Butler KL, Best IM. Endometrioma of the abdominal wall. Am J Obstet Gynecol. 2002;187:1709-1710.
- Goel P, Sood S S, Romilla, Dalal A. Cesarean scar endometriosis - Report of two cases. Indian J Med Sci. 2005;59:495-498.
- Nirula R, Greaney GC. Incisional Endometriosis: An Underappreciated Diagnosis in General Surgery. Journal of American college of surgeons. J Am Coll Surg. 2000;190:404-407.
- Cihangir Uzunçakmak, Ahmet Gülda G, Hasene Özçam, Kemal Dinç. Scar Endometriosis: A Case Report of This Uncommon Entity and Review of the Literature. Case Reports in Obstetrics and Gynecology Volume 2013, Article ID 386783.
- Balleyguier C, Chapron C, Chopin N, Helenon O, Menu Y. Abdominal wall and surgical scar endometriosis. results of magnetic resonance imaging. Gynecol Obstet Invest. 2003;55:220-224.
- Pathan SK, Kapila K, Haji BE, Mallik MK, Al-Ansary TA, George SS, et al. Cytomorphological spectrum in scar endometriosis: a study of eight cases. Cytopathology. 2005;16(2):94-99.
- Crum CP. The female genital tract. In: Cotran RS, Kumar V, Collins V, (eds). Robbins Pathologic Basis of Disease. Saunders, Philadelphia, Pa, USA, 6th edition, 1999.
- Meti S, Wiener JJ. Scar endometriosis-a diagnostic dilemma, European Clinics in Obstetrics and Gynaecology. 2006;2:62-64.
- Patterson GK,Winburn GB. Abdominal wall endometriomas: report of eight cases. American Surgeon. 1999;65:36-39.
- Rivlin ME, Das SK, Patel RB, Meeks GR. Leuprolide acetate in the management of cesarean scar endometriosis. Obstet Gynecol. 1995;85(5 Pt 2):838-839.
- Wasfie T, Gomez E, Seon S, Zado B. Abdominal wall endometrioma after cesarean section: a preventable complication. Int Surg. 2002;87:175-177.
- Rani PR, Soundararaghavan S, Rajaram P. Endometriosis in abdominal scars-review of 27 cases. International Journal of Gynecology and Obstetrics. 1991;36:215-218