Introduction
Mitral valve prolapse (MVP) occurs when the belly of leaflets extends 2 mm above the plane of the mitral annulus during ventricular systole. It is the most common cardiac valvular anomaly in developed countries. Myxomatous degeneration is the main etiology of prolapsing valvular leaflets causing mitral regurgitation, explaining the fact that MVP is uncommon before adolescence. Indeed, the prevalence of MVP was 0.7% in a population of healthy teenagers [
2]. According to the classification by Carpentier et al. [
3], the free edge of the posterior leaflet is divided into three scallops: P1 (lateral); P2 (middle); and P3 (medial). The anterior leaflet is subdivided into A1, A2 and A3 regions that are opposite the scallops of the posterior leaflet. Prolapse of the posterior leaflet (PPL) currently represents the most common cause of mitral regurgitation in Western population and was the first lesion accessible for repair [
4].
Case Report
A 23 year old male nonsmoker, nonalcoholic with no history of familial coronary artery disease presented with effort intolerance NYHA class III over last 3 months to the Cardiology outpatient department of AIIMS, Bhubaneswar associated with exertional palpitation, atypical chest pain and easy fatigability. There was no history of antecedent fever, rash and arthralgia. His infancy and childhood days were uneventful. He did not reveal any history of classical angina, syncope, orthopnea or paroxysmal nocturnal dyspnea. There was no history suggestive of rheumatic fever in early childhood. Clinical examination revealed high volume non-collapsing pulse, cardiomegaly with ill sustained apex, non-ejection click and a late systolic murmur grade III/VI accentuated with standing and Valsalva maneuverer. Serum chemistries including glucose, lipid panel and renal profile were within normal limit. ESR, CRP and ASO titre were within normal limit. ECG revealed left atrial enlargement and left ventricular hypertrophy with diastolic overload pattern and small S wave in V1.
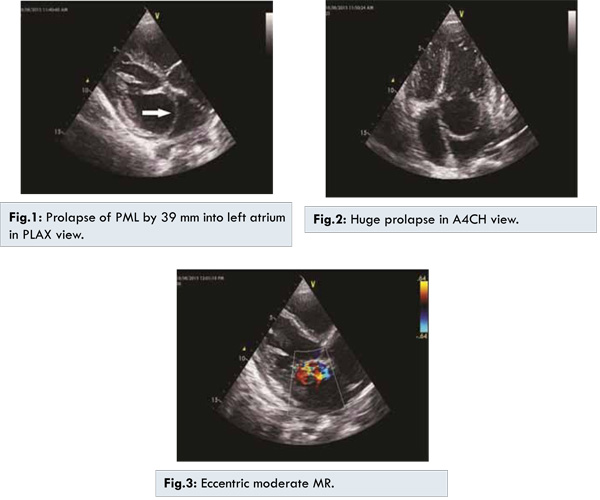
Echocardiogram revealed 39 mm prolapse [Fig.1] of P2 segment of posterior mitral leaflet (PML) into left atrium (LA) in PLAX view with moderate eccentric mitral regurgitation (MR) (jet area 5.2 cm2) [Fig.3], both anterior mitral leaflet (AML) and PML were thick (6 mm). Patient was advised to undergo mitral valve repair. The goal of the surgical community is always 100% repair of prolapsing posterior leaflet. With midline sternotomy and under CPB, tailored and limited resection of posterior leaflet was done ensuring a regular and non-prolapsing leaflet. Post-procedure, there was no residual mitral regurgitation as revealed by echocardiography, patients dyspnea abated and there was perfect apposition of both leaflets.
In our case, tailored resection of mitral valve was needed because of unusual huge prolapse of PML. Although it was a tough journey by the cardiac surgeon to repair such a huge prolapse, the patient was albeit saved from the morbidity of a mechanical prosthesis including anticoagulation. The repair of PPL, guided by anatomical considerations, should become a patient-specific spectrum of techniques ranging from respect to resect. Post-repair patient is doing fine at present.
Discussion
Our case was unique because of the fact that such a huge prolapse of PML is more than that 37 mm ever described in literature [
1]. Patient was symptomatic, because such a huge prolapse of PML into LA with mitral regurgitation increased left atrial pressure with resultant pulmonary venous congestion. Subacute myxomatous degeneration of mitral valve leaflet may have increased the degree of prolapse, compromising the left atrial volume and increasing pressure explaining the subacute onset of effort dyspnea in this patient. Eccentric mitral regurgitation may have been underestimated in this patient as the jet was along with anterior mitral leaflet towards the interatrial septum. Huge prolapse of PML like ours also occurs in Marfan syndrome. Such a huge mitral valve prolapse if someone encounters in young, rheumatic carditis is never taken into account; rather to think of myxomatous valve degeneration. If young person, healthy one presenting with chest pain, palpitation or shortness of breath, MVP stands out as a close differential diagnosis [
5]. Repair of the valve will reverse the natural story of mitral regurgitation in those patients. Always respect the valve but do not resect and replace the valve in young if possible is the dictum [
6]. Mitral valve repair for posterior prolapse is a low-risk, durable surgical procedure that address both leaflet and annulus. At 10 years, freedom from mitral reoperation is almost 97%, and 77% for having no or 1+ MR; 11% for having 3+ or 4+ MR [
7]. Most common modality of mitral valve repair is quadrangular resection with annuloplasty. Recurrent MR that is moderately severe or severe is uncommon in the decade after operation and early repair addresses a complete repair. Mitral repair affords superior long-term survival, with permanence comparable with mechanical valve replacement [
8]. Conservative surgery with Carpentier’s techniques is feasible in the majority of cases of congenital mitral valve insufficiency. This technique offers stable long-term results with a low rate of reoperation [
9]. Chordal shortening and transfer remains the technique for AML repair whereas triangular resection remains the favorite for degenerative MR [
10]. Although tailored resection and reconstruction of this huge prolapsing PML was quite tedious for our cardiac surgeon, ultimately we achieved a healthy repair with no residual resurge.
Conclusion
39 mm huge prolapse of PML is a rarest entity never described in literature. Ours is unique in eliciting such a huge prolapse of PML secondary to myxomatous degeneration. Repair is always the age respected golden option across whole spectrum of valvular diseases when anatomy favors it. With tedious resection and repair by our cardiac surgeon, we achieved a well apposing valve with no residual regurgitation. This rare entity teaches us myxomatous degeneration can make the bellies of the leaflet so weak that such a huge prolapse can happen with intact chordae and it reminds us the age old teaching: always try to repair the valve, not to replace it.
References
- Sattur S, Bates S, Movahed MR. Prevalence of mitral valve prolapse and associated valvular regurgitations in healthy teenagers undergoing screening echocardiography. Exp Clin Cardiol. 2010;15:e13-15.
- Sahn JD, Allen HD, Friedman AF, Goldberg S. Mitral Valve Prolapse in Children: A Problem Defined by Real-time Cross-sectional Echocardiography.Circulation. 1976;53:651-657.
- Carpentier A, Branchini B, Cour JC, Asfaou E, Villani M, Deloche A, et al. Congenital malformations of the mitral valve in children. Pathology and surgical treatment. J Thorac Cardiovasc Surg. 1976;72:854-866.
- Perier P, Hohenberger W, Lakew F, Batz G, Diegeler A. Minimally invasive repair of posterior leaflet mitral valve prolapse with the “respect” approach. Ann Cardiothorac Surg. 2013;2(6):833-838.
- Franca H. An Interpretation-Mitral Valve Prolapse Syndrome. Arq Bras Cardiol volume 74, (nº 5), 2000 pp 456-458.
- Perier P, Hohenberger W, Lakew F, Batz G, Urbanski P, Zacher M, et al. Toward a new paradigm for the reconstruction of posterior leaflet prolapse: midterm results of the “respect rather than resect” approach. Ann Thorac Surg. 2008;86:718-725.
- Johnston DR, Gillinov AM, Blackstone EH, Griffin B, Stewart W, Sabik JF, et al. Surgical repair of posterior mitral valve prolapse: implications for guidelines and percutaneous repair. Ann Thorac Surg. 2010;89(5):1385-1394.
- Suri RM, Schaff HV, Dearani JA, Sundt TM , Daly RC, Mullany CJ, et al. Survival advantage and improved durability of mitral repair for leaflet prolapse subsets in the current era. Ann Thorac Surg. 2006;82(3):819-826.
- Chauvaud S, Fuzellier JF, Houel R, Berrebi A, Mihaileanu S, Carpentier A. Reconstructive surgery in congenital mitral valve insufficiency (Carpentier’s techniques): long-term results. J Thorac Cardiovasc Surg. 1998;115(1):84-93.
- Smedira NG, Selman R, Cosgrove DM, McCarthy PM, Lytle BW, Taylor PC, et al. Repair of anterior leaflet prolapse: chordal transfer is superior to chordal shortening. J Thorac Cardiovasc Surg. 1996;112(2):287-292.