Introduction
Plasma cell gingivitis is dense plasma cell infiltration in the gingiva secondary to hypersensitive reaction [
1,
2]. It may clinically present as isolated nodule (granuloma) or involve the whole gingiva [
3]. Plasma cell infiltration is also found in other organs of the system like the lung, bronchi, liver, kidney, spinal cord, intracranial space, thyroid gland and stomach. When reported in mucous membranes like the oral cavity, upper aerodigestive tract or glans penis, it is known as plasma cell mucositis [
4]. Bhaskar et al. first gave a detailed description of the lesion in the gingiva complete with histopathological examination [
3]. This entity showed predominance in the 1940s and 1950s and later resurgence in 1980s secondary to the use of flavored chewing gum [
5,
6]. The extramedullär/plasmacytoma was described as a solitary, well defined, locally destructive lesion usually confined to the mucosa of the oropharyngeal region [
7]. Plasma cell gingivitis is also known as atypical gingivostomatitis, allergic gingivostomatitis, unusual gingivostomatitis and idiopathic gingivostomatitis [
8].
Diagnosis is important to differentiate it from a variety of conditions namely extramedullary plasmacytoma, discoid lupus, cicatricial pemphigoid, leukemia and HIV gingivitis. The predominant underlying reaction appeared to be hypersensitivity due to a variety of agents used in chewing gums or toothpastes, like mint, cinnamon, cloves, cardamom, red chilli peppers, khat, colocasia leaves or even prophy pastes like pumice [
2,
9-
13]. Many a times these cases were associated with chelitis, glossitis or psoriasis. Histopathologically, amplification in the number of mature plasma cells in the lamina propria is seen. Plasma cell gingivitis can be classified into 3 types: caused by an allergen, bearing a neoplastic nature and gingivitis of unknown origin [
14]. Though benign, lesions of plasma cell gingivitis occasionally mimic acute leukemia clinically and multiple myeloma or extramedullary plasmacytoma histologically. Hence, the diagnosis requires hematological screening in addition to clinical and histopathological examinations to rule out malignant conditions. Plasma cell gingivitis is purely benign, and the detection and elimination of the exposure to the antigenic agent will bring about the remission of the condition. However, the allergen in most cases is unknown, despite extensive allergy testing. Here we have presented a rare case of plasma cell gingivitis caused due to herbal toothpaste associated with generalized aggressive periodontits.
Case Report
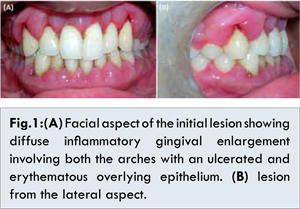
A 26 year old male patient presented to the outpatient department of Periodontics and Oral Implantology, Dr. R Ahmed Dental College & Hospital, Kolkata with the chief complaints of swelling and bleeding from gums for the past 8 months. Clinical examination revealed diffuse gingival enlargement in both the arches covered by an erythematous epithelium. The enlargement was reddish pink in color, soft and edematous in consistency, with rounded gingival margins [Fig.1A,B]. The enlargement involved only the marginal and attached gingiva and did not progress beyond mucogingival junction. A pocket probing depth of 5-7 mm was recorded on an average. Systemic history was insignificant. The patient replied in the negative for a history of drugs like calcium channel blockers, antiepileptics or immunosuppressants which are known to cause gingival enlargement. On probing further, the patient revealed the use of herbal toothpaste for a year but had discontinued it a month ago. Analysis of the contents showed this paste contained mint and clove which could be possible allergens. The patient was given strict instructions to stay away from the product till a definite diagnosis was achieved.
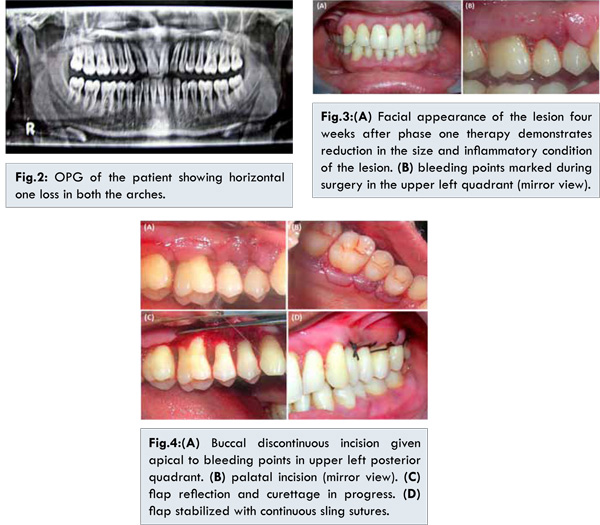
The OPG revealed generalized horizontal bone loss, about one third in both the arches [Fig.2]. The preliminary treatment comprised of oral hygiene instructions followed by scaling and root planing. The patient was advised to use a mouthrinse of 0.2%, 10 mL chlorhexidine twice daily along with the use of an ultrasoft toothbrush and dental floss. A blood investigation was advised to rule out leukemia or any other blood dyscrasias. The patient was asked to report back after two weeks. Proper home care and the use of chlorhexidine mouthwash reduced inflammation after four weeks [Fig.3A,B]. The enlargement though was still persistent and appeared to have a fibrotic component. Blood reports revealed no abnormalities. The patient showed visible improvement after the discontinuation of the herbal toothpaste and regular follow ups reinforcing oral hygiene. Gingival contours, though were not completely re-established and the tissue was surgically removed using undisplaced flap technique after six weeks [Fig.4A,D]. Healing was uneventful. The patient was followed up for two years. No recurrence was noted during that period.
Histology revealed plasma cells densely infiltrating the fibrocollagenous tissues, epithelial hyperplasia, elongated rete pegs, intact basement membrane and no cellular atypia [Fig.5]. Immunohistochemistry with CD34, CD43, CD44, CD117, Ki-67, kappa and lambda light chain antibodies were performed. A strong positive reactivity was observed for kappa light chain [Fig.6A] in the polyclonal plasma cells. Polyclonal plasma cell population showed no reactivity with lambda light chain [Fig.6B]. The kappa/lambda ratio less than 10:1 was observed. Interestingly, plasma cells showed CD34-, CD43-, CD117-, Ki67- and CD44+ reactivity [Fig. 6C-H].
Discussion
Plasma cell gingivitis is a reactive, polyclonal and benign lesion, and has to be crucially differentiated from other malignant or pre-malignant monoclonal lesions like multiple myeloma or Waldenstrom’s macroglobulinemia or plasmacytoma [
12,
15]. Unlike plasmacytomas, the basic proliferative process associated with the growth of plasma cell gingivitis is reactive plasmacytic proliferation. It may be focal when the allergen is localized or diffuse when generalized. The present case was very similar to plaque induced gingivitis which involves marginal and papillary gingiva but this lesion involved whole gingiva upto the mucogingival junction. A negative Nikolsky’s sign ruled out pemphigus, other cutaneous diseases like pemphigoid, lichen planus and discoid lupus erythematosus.
The immunohistochemistry study further confirmed the polyclonality of this lesion with the aid of kappa and lambda light chain reactivity. It was observed that activation of plasma cell induced the expression of CD molecules during the malignant transformation, we have systematically introduced five more markers. The CD34, CD43, CD117 and Ki67 markers which are positively stained in neoplastic cells, were negatively stained in this case. Simultaneously it was found that the plasma cells stained positive for CD44, which was reported to be essential for the physiologic activities of normal cells and pathologic activities of neoplastic cells. In correlation with the negative staining results for CD34, CD43, CD117 and Ki67, CD44 expression likely suggested to be facilitating the development of plasma cells into terminally differentiated cells [16]. Hence CD44-/+ with CD34-, CD43-, CD117- and Ki67- may be one of the future biological markers to be implemented in distinguishing the neoplastic or non-neoplastic nature of these lesions. Though the etiology could not be confirmed precisely, discontinuing the toothpaste proved to be beneficial.
Conclusion
This was a case of plasma cell gingivitis associated with generalized aggressive periodontits due to the regular use of herbal toothpaste. Moreover, present case report first time suggested the significant use of CD34, CD43, CD117, Ki67 and CD44 molecules for the differentiation of plasma cell gingivitis from malignancies. As well the successful management of present case since the gingiva did not shrink on its own and moderate attachment loss was present, flap surgery played an important role.
References
- Regezi JA, Sciubba JJ. Oral pathology: clinical pathologic correlations. Philadelphia: WB Saunders. 1989;145.
- Serio FG, Siegel MA, Slade BE. Plasma cell gingivitis of unusual origin. A case report. Journal of periodontology. 1991;62:390-393.
- Bhaskar SN, Levin MP, Frisch J. Plasma cell granuloma of periodontal tissues. Report of 45 cases. Periodontics. 1968;6:272.
- Smith ME, Crighton AJ, Chisholm DM, Mountain RE. Plasma cell mucositis: a review and case report. Journal of Oral Pathology & Medicine. 1999;28:183-186.
- Miller J. Cheilitis from sensitivity to oil of cinnamon present in bubble gum. Journal of the American Medical Association. 1941;116:131-132.
- Palmer RM, Eveson JW. Plasma-cell gingivitis. Oral Surgery, Oral Medicine, ral Pathology. 1981;51:187-189.
- Poswillo D. Plasmacytosis of the gingiva. British Journal of Oral Surgery. 1967;5:194-202.
- Silverman Jr S, Lozada F. An epilogue to plasma-cell gingivostomatitis (allergic gingivostomatitis). Oral Surgery, Oral Medicine, Oral Pathology. 1977;43:211-217.
- Kerr DA, McClatchey KD, Regezi JA. Allergic gingivostomatitis (due to gum chewing). Journal of Periodontology. 1971;42:709-712.
- Allen CM, Blozis GG. Oral mucosal reactions to cinnamon-flavored chewing gum. The Journal of the American Dental Association. 1988;116:664-667.
- Bali D, Gill S, Bali A. Plasma cell gingivitis-A rare case related to Colocasia (arbi) leaves. Contemporary Clinical Dentistry. 2012;3:S182.
- Peacock ME, Hokett SD, Hellstein JW, Herold RW, Matzenbacher SA, Scales DK, et al. Gingival plasma cell granuloma. Journal of Periodontology. 2001;72:1287-1290.
- Marker P, Krogdahl A. Plasma cell gingivitis apparently related to the use of khat: report of a case. British Dental Journal 2002;192:311-313.
- Imran F, Rajan S, Vijay G. A Case of Plasma Cell Granuloma of Unknown Cause. Journal of Orofacial Research. 2012;2:235-237.
- Macleod RI, Ellis JE. Plasma cell gingivitis related to the use of herbal toothpaste. British Dental Journal 1989;166:375-376.
- Minges Wols HA. Plasma cells. eLS 2006. Available from http://onlinelibrary.wiley.com/doi/10.1002/9780470015902.a0004030.pub2/full. Accessed on July 2, 2015.