Introduction
Diffuse toxic goiter a common autoimmune thyroid disease, usually presents with clinical features of thyrotoxicosis. Hurthle cell carcinoma is an unusual and relatively rare type of differentiated thyroid cancer, a variant of follicular carcinoma. This accounts for only about 3%-10% of all differentiated thyroid cancers. Paraneoplastic neurologic syndromes are often immune related, associated with antibodies against neural antigens expressed by the tumor [
2]. Classical PNS include paraneoplastic limbic encephalitis (PLE), subacute sensory neuronopathy (SSN), paraneoplastic cerebellar degeneration (PCD), and paraneoplastic opsoclonus - myoclonus (POM), as well as Lambert - Eaton myasthenic syndrome (LEMS) and paraneoplastic peripheral nerve hyperexcitability (PPNH) [
2].
Here we present one lady who suffers from diffuse toxic goiter and coexisting Hurthle cell carcinoma of thyroid with distant metastasis, who presented with progressive asymmetric lower limb weakness, and was diagnosed as mononeuritis multiplex.
Case Report
67 year old lady presented to our hospital with diffuse body pains and progressive weakness of lower limbs of 2 months. She needed support of two persons to stand or walk to the toilet and was not able to sit unsupported in bed. She experienced easy tiredness and weight loss during the preceding 6 months. There is history of painless swelling of right lobe of thyroid gland for last 2 years, slowly increasing in size with no pressure symptoms. On questioning she admits numbness in both feet. No weakness of upper limbs, bladder dysfunction, symptoms related to cranial nerves or cardiorespiratory symptoms were elicited.
She was moderately built and nourished, diffuse nodular goiter with largest nodule of about 5 cm size in right lobe, not fixed to nearby structures and no enlarged lymph nodes in neck. Her hands were warm and there was fine tremor, No eye signs of Graves’ disease were elicited. Pulse rate was 100/minute, high volume and BP 180/90mm Hg, afebrile. No signs detected over heart, chest or abdomen. Neurological examination showed predominant weakness of hip flexors (grade 3/5) and knee extensors (grade 1/5 right and grade 2/5 left side) and grade 4/5 for muscles acting at ankle joints, right lower limb was weaker than left side. Touch and pain sensation were less appreciated on distal parts of both feet. All deep tendon reflexes were sluggish and plantar flexor on both sides.
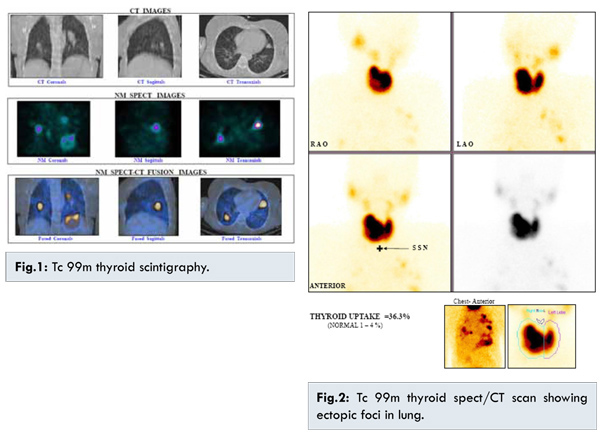
Free T4: 41.33 (9.0-20 pmol/L), Free T3: 8.6 (4-8.3 pmol/L) and TSH: <0.05 (0.25-5 µIU/mL) suggested severe thyrotoxicosis. Other routine investigations were CBC, renal and liver functions normal, ESR 23 mm, calcium 9 mg/dL, creatine kinase 35 U/L (24-170 U/L). Ultrasound of neck showed multiple varying sized nodules with varying echogenicity, largest 4x2.7 cm in right lobe with increased peripheral and central vascularity and level II cervical lymph nodes. Thyroid scintigraphy (Tcm99) [Fig.1,2] showed hyperactive diffuse toxic goiter with a large ill-defined intrathyroidal cold nodule in the right lobe and multiple focal extrathyroidal functioning thyroid tissues in both lungs with impression of well differentiated carcinoma of thyroid involving right lobe with multiple lung metastasis (tracer uptake by thyroid gland 36.3%).
CT scan of neck showed a large heterogeneously enhancing nodule in right lobe, enlarged level II lymph nodes and lung metastasis. FNAC revealed cellular aspirate with sheets of uniform oncocytic cells and follicular cells arranged as sheets suggestive of Hurthle cell neoplasm. Clinical diagnosis was lumbar plexopathy with a possibility of mononeuritis multiplex. Nerve conduction studies (NCS) showed reduced CMAP amplitude, with right more than left peroneal nerve, inelicitable femoral CMAP and normal response for sural nerves and upper limb nerves, consistent with multiple peripheral nerve lesions. CSF study, MRI lumbosacral spine with lumbar plexus study were normal.
Final diagnosis was diffuse toxic goiter/ Hurthle cell neoplasm with pulmonary metastasis/ lower limb weakness due to mononeuritis multiplex, likely a paraneoplastic neurologic syndrome. She was treated with intravenous methyl-prednisolone for 5 days followed by oral steroids, high dose carbimazole and physiotherapy. Over 4 weeks power improved in both lower limbs and she was able to sit unsupported and walk with support (power of hip flexor improved to grade 4, knee extensor to grade 3 on right side and grade 4 on left side). Once euthyroid she underwent total thyroidectomy with central compartment neck dissection.
Thyroidectomy specimen with a fleshy nodule measuring 5x4 cm revealed a fleshy, grey white growth invading the capsule. Microscopy showed a poorly differentiated neoplasm with predominant follicular pattern. Insular pattern and small foci of papillary and Hurthle cell areas with anisonucleosis areas of vascular invasion of capsule and focal areas of necrosis were noted [Fig.3,4].
Post-operative serum calcium was 7.3 mg/dL, serum T4: 11.0, T3: 1.8, TSH: < 0.05 on 10th day (off neomercazole and thyroxine following surgery). High normal values for thyroid hormones may be the result of functioning metastasis. She was advised high dose radioiodine ablation but she has not turned for follow up.
Discussion
Graves’ disease is characterized by diffuse toxic goiter and thyrotoxicosis, it may be accompanied by ophthalmopathy and occasionally by dermopathy. Nervous system manifestations are common and include nervousness, emotional lability and hyperkinesia. Thyrotoxic myopathy is a rare presentation with predominant weakness and wasting of proximal muscles of limbs, affects often men and may overshadow other clinical features, correlates with thyroid hormone levels and may resolve after successful therapy. In our patient we first considered this possibility, as she was overtly thyrotoxic and untreated for several months. NCS results and asymmetric weakness of lower limbs are consistent multiple peripheral nerve lesions and not suggestive of thyrotoxic myopathy.
Mononeuritis multiplex is an asymmetric asynchronous sensory and motor neuropathy involving isolated damage to at least two separate non-contiguous nerve trunks, not a true distinct disease entity [
3]. The common causes include diabetes mellitus [
4], multiple nerve compressions, systemic necrotizing vasculitis [
5], connective tissue disorder, infectious causes like HIV, leprosy and other causes like amyloidosis [
6] and paraneoplastic syndromes [7]. The cause may not be identified in one third of patients. Classical para-neoplastic syndromes include paraneoplastic limbic encephalitis (PLE), subacute sensory neuronopathy (SSN), paraneoplastic cerebellar degeneration (PCD), and paraneoplastic opsoclonus-myoclonus (POM), as well as Lambert-Eaton myasthenic syndrome (LEMS) and paraneoplastic peripheral nerve hyperexcitability (PPNH) [
2]. In solid tumors, the common neurological syndromes are myasthenia gravis, which occurs in 15% of patients with a thymoma, and LEMS, which affects 3% of patients with SCLC (lung). For other solid tumors, the incidence of PNS is <1%. Clinical syndromes are never pathognomonic for a paraneoplastic etiology, and a high index of clinical suspicion is required [
8].
Hurthle cell carcinoma is a variant of follicular carcinoma which accounts for nearly 3% of thyroid cancers, prognosis is less favorable to other differentiated cancers of thyroid gland. In a study of 28 patients with Hurthle cell neoplasms of which 19 were malignant, and having distant metastasis during presentation, no paraneoplastic manifestations were described [
9]. A case report by Bier et al. reported a 71 year old woman with papillary carcinoma of thyroid presenting with SIADH [
10]. Kalliabakos reported 31 year old patient who presented with polymyositis along with papillary carcinoma of thyroid [
11]. Case reported by Hyar et al. describes a woman with papillary carcinoma of thyroid and paraneoplastic myoclonus [
2].
The first goal of treatment of paraneoplastic syndrome (PNS) is control of primary tumor, antitumor therapy may halt deterioration of PNS. Immunotherapy consisting of plasma exchange, steroids, and intravenous immunoglobulins is ineffective in most cases [
12].
Conclusion
We report possible paraneoplastic syndrome in form of progressive asymmetrical lower limb weakness in a case of Hurthle cell carcinoma of thyroid in which nerve conduction studies were consistent with mononeuritis multiplex.
References
- Pelosof LE, Gerber DE. Paraneoplastic Syndromes: An approach to Diagnosis and Treatment. Mayo Clin Proc. 2010;85(9):838-854.
- Graus F, Delattre JY, Antoine JC, Dalmau J, Giometto B, Grisold W, et al. Recommended diagnostic criteria for paraneoplastic neurological syndromes. J Neurol Neurosurg Psychiatry. 2004;75:1135-1140.
- Parry GJ. Mononeuropathy multiplex (AAEE case report #11) Muscle Nerve. 1985;8(6):493-498.
- Kelkar P, Parry GJ. Mononeuritis multiplex in Diabetes Mellitus: evidence for underlying immune pathogenesis. Journal of Neurology Neurosurgery Psychiatry. 2003;74(6):803-806.
- Gorson KC. Vasculitic neuropathies: an update. Neurologist. 2007;13(1):12-19.
- Tracy JA, Dyck PJ. Primary amyloidosis presenting as upper limb multiple mononeuropathies. Muscle Nerve. 2010;41(5):710-715.
- Leypoldt F. Friese MA, Bohm J, Baumer T. Multiple enlarged nerves on neurosonography: an unusual paraneoplastic case. Muscle Nerve. 2011;43(5):756-758.
- Janet W. de Beukelaar, Peter A. Sillevis Smitt. Managing Paraneoplastic Neurological Disorders. The Oncologist. 2006;11:292-305.
- Barnabei A, Ferretti E, Baldelli R, Procaccini A, Spriano G, Appetecchia M. Hurthle cell tumors of thyroid. Personal experience and review of literature. Acta Otorhinolaryngol Ital. 2009;29(6):305-311.
- Beier F, Moleda L, Guralnik V, Hahn P, Schardt K, Andreesen R, et al. Papillary thyroid cancer associated with syndrome of inappropriate antidiuresis: a case report. Journal of Medical Case Reports. 2010;4:110.
- Kalliabakos D, Pappas A, Lagoudianakis E, Papadima A, Chrysikos J, Basagiannis C. A case of polymyositis associated with papillary thyroid cancer: a case report. Cases Journal. 2008;1:289.
- Keime-Guibert F, Graus F, Fleury A, René R, Honnorat J, Broet P, et al. Treatment of paraneoplastic neurological syndromes with antineuronal antibodies with a combination of immunoglobulins, cyclophosphamide and methylprednisolone. Journal of Neurology Neurosurgery Psychiatry. 2000:68:479-482.