Introduction
Subcapsular liver hematoma (SLH) has been reported in less than 2% of pregnancies complicated by HELLP syndrome (hemolysis, elevated liver enzymes, and low platelets) and preeclampsia, leading to increased rate of both maternal and perinatal morbidity and mortality [
1,
2]. The SLH may present as right upper quadrant abdominal pain or shoulder pain, abdominal distension, nausea or vomiting. SLH may lead to life threatening complications such as disseminated intravascular coagulation (DIC), acute liver, and kidney failure due to hepatic rupture. We discuss the SLH secondary to severe pre-eclampsia and review the literature.
Case Report
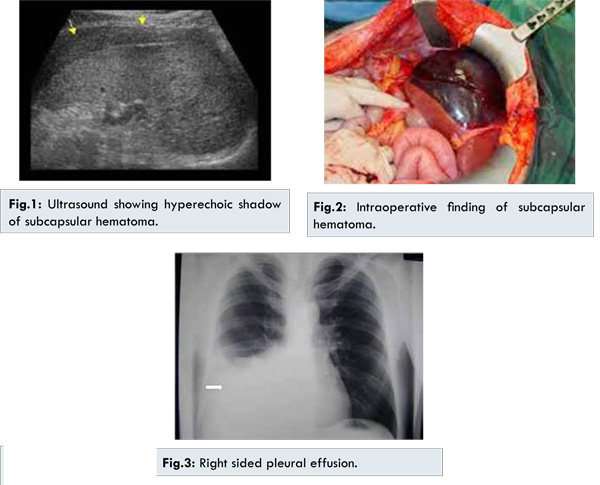
A 30-year-old woman, gravida 3, abortion 2, was admitted at 34 weeks of gestation with impending eclampsia. The patient’s complaints were frontal headache and visual impairment. Her arterial blood pressure was 160/100 mmHg. Laboratory findings revealed urine albumin 2+, serum bilirubin 2.4 mg/dL, serum aspartate amino transaminase (AST): 247 IU/L (N: 5-34), serum alanine amino transaminase (ALT): 212 IU/L (N: 0-55), serum urea 50 mg/dL and creatinine 1.2 mg/dL, hemoglobin (Hb): 10.4 mg/dL (N: 11.5-16.0), and platelet count (Plt): 60,000/mm3 (N:1,50,000-4,50,000). In obstetrical ultrasonography (USG), average gestational age of 34 weeks with 2 kg baby weight was calculated. Lower segment Caesarean section (LSCS) was done in view of unfavorable cervix with fetal intrauterine growth retardation. Intraoperative, 100 mL of hemorrhagic fluid was suctioned, hemostasis achieved, and patient shifted to postoperative ward for monitoring. One hour postoperatively, patient went into shock with no palpable pulse and 40 mmHg systolic blood pressure. Dopamine and blood transfusion were administered to maintain vitals. Urgent ultrasound confirmed the hemorrhagic fluid collection in abdomen and hyperechoic shadow of subscapular liver hematoma was seen [Fig.1]. Emergency laparotomy showed healthy uterine wound with no bleeder. However, fresh blood was accumulating in right colonic gutter. Incision was extended to xiphisternum and large clot appreciable over anterior surface of liver was gently removed [Fig.2]. An actively bleeding 9 cm transverse tear was present on anterior surface that was compressed with mop for 10 minutes, hemostatic material kept and abdomen closed with drains in subhepatic and pouch of Douglas. Multiple blood transfusions, antihypertensives and antibiotics were administered postoperatively. Follow up investigations at 24 hours showed hemoglobin: 8.3 gm%, INR 1.0, platelet: 73,000/cumm, bilirubin: 0.90 mg%, blood urea: 96 mg%, serum creatinine: 2.3 mg%, SGOT: 340 IU/mL and SGPT: 100 IU/mL. Intravenous furosemide was started in view of oliguria. Over next 48 hour pulse rate settled down near 100/min with normal blood pressure, 500 ml subhepatic drain output and maintained urine output. Sudden onset breathlessness on day 6 secondary to pleural and pericardial effusion was managed conservatively [Fig.3]. Over the time, drain output reduced and drain was removed by 20 and 25 day respectively. Liver enzyme, kidney function came to normal after 4 weeks. Patient was discharged on antihypertensive therapy.
SLH in pregnancy was reported firstly by Abercombie in 1844 [
3]. SLH, a rare complication of preeclampsia and HELLP, occurs in about 1-2% of all preeclampsia cases and HELLP syndrome [
1,
2]. The incidence of SLH has been reported to be higher in the group of advanced maternal age and multiparous patients [
5]. The underlying pathogenesis of SLH in HELLP syndrome has been reported due to fibrin deposition, hypovolaemia, hepatic ischaemia, and infarction causing haemorrhage and SLH [
6]. Expansion of the SLH secondary to traumatic conditions like abdominal palpation, patient transportation, manual removal of the placenta, uterine contractions, and vomiting can induce rupture of hepatic capsule [
6]. Periportal or focal parenchymal necrosis and bleeding under Glisson capsule have frequently been observed in SLH [
7-
9].
SLH in pregnancy must be followed up with hemodynamic or coagulation profile and imaging during the management of HELLP syndrome or/and preeclampsia. Hemodynamically stable patients should be followed up conservatively by means of intensive medical support with fluid and electrolyte management, blood transfusion, and treatment of HELLP syndrome or/and preeclampsia. The administration of recombinant factor VIIa, hemostatic mesh and suturing of omentum to bleeding surface may be useful to stop hemorrhage and to avoid surgery in patients not responsive to surgical therapy [
6,
10]. If rupture occurs and the patient is unstable hemodynamically, surgery may be required. When the hemorrhage cannot be controlled with conservatively or with surgical techniques and acute liver failure occurs, liver transplantation should be considered [
11]. Sibai reported a 13-year retrospective review of three patients with SLH. Two of them were managed conservatively and discharged from hospital. The other patient underwent hepatic resection and had mortality due to multiple organ failure [
12]. In another study, Wicke et al. reported a review of 5 patients with subcapsular liver hematoma [
13]. Three patients of them were managed conservatively and two required urgent surgical intervention, one of whom required liver transplantation
Conclusion
Subcapsular liver hematoma with HELLP syndrome and severe preeclampsia is a rare clinical entity and should be suspected in signs of clinical symptoms. Vigilant monitoring of these patients with HELLP syndrome by advanced imaging techniques in pre- and postpartum period is mandatory. If the patient’s vital signs are unstable, surgical management should be the first choice of treatment.
References
- van Dyke RW. The liver in pregnancy. In: Hepatology: A TextBook of Liver Disease. 2nd Edition. Churchil Livingstone; New York:1996. pp.1132-1135.
- Westengaard L. Spontaneous rupture of the liver in pregnancy. Acta Obstet Gynecology. 1983;59:559-561.
- Abercrombie J. Case of hemorrhage of the liver. London Medical Gazette. 1844;34:792-794.
- Bis KA, Waxman B. Rupture of the liver associated with pregnancy: a review of the literature and report of 2 cases. Obstetrical and Gynecological Survey. 1976;31:763-773.
- Ferri FF. Ferri’s Clinical Advisor. Mosby, Elsevier: Philadelphia, Pa; USA, 2012.
- Dessole S, Capobianco G, Virdis P, Rubattu G, Cosmi E, Porcu A. Hepatic rupture after cesarean section in a patient with HELLP syndrome: a case report and review of the literature. Archives of Gynecology and Obstetrics. 2007;276(2):189-192.
- Robbins S, Cotran RS, Kumar V. Pathologic Basis of Disease, 3rd edition, 1984.
- Kapana M, Evsenb MS, Gum¨ us M, Onder A, Tekbas G. Liver hematoma in HELLP syndrome: case report. Gastroenterology Research. 2010;3(3):144-146.
- Anthony J, Johanson R, Dommisse J. Critical care management of severe pre-eclampsia. Fetal and Maternal Medicine Review.1994;6(4):219-229.
- Carlson KL, Bader CL. Ruptured subcapsular liver hematoma in pregnancy: a case report of nonsurgical management. American Journal of Obstetrics and Gynecology. 2004;190(2):558-560.
- Barton JR, Sibai BM. Care of the pregnancy complicated by HELLP syndrome. Gastroenterology Clinics of North America.1992;21(4):937-950.
- Sibai BM. The HELLP syndrome (Hemolysis, elevated liver enzymes, and low platelets): much ado about nothing? American Journal of Obstetrics and Gynecology. 1990;162(2):311-316.
- Wicke C, Pereira PL, Neeser E, Flesch I, Rodegerdts EA, Becker HD. Subcapsular liver hematoma in HELLP syndrome: evaluation of diagnostic and therapeutic options-a unicenter study. American Journal of Obstetrics and Gynecology. 2000;190(1):106-112.