Introduction
Endoscopic retrograde cholangiopancreatography (ERCP) is a minimally invasive procedure for the diagnosis and treatment of biliopancreatic system diseases. Although it is minimal invasive procedure, it has some complications that may cause mortality even if done by expert [
1]. Most common complications related to ERCP are pancreatitis, cholangitis, perforation and bleeding due to the papillotomy [
2]. Complications related to this procedure vary from 2.5% to 8%, with a mortality rate of 0.5% to 1% [
3-
4]. Subcapsular hepatic hematomaafter ERCP is extremely uncommon and was firstly described in 2000 [
5]. Since then more than 20 cases were reported in the literature [
3], and just one of them is from Turkey [
6]. Here we report an unusual case of post-ERCP hepatic subcapsular hematoma.
Case Report
A 55 year-old man with a medical history of cholelithiasis and chronic obstructive pulmonary disease was admitted to general surgery clinic for right upper quadrant pain with elevated transaminase and bilirubin levels. He was not using any anticoagulant or anti-aggregant drug. The common bile duct stone was diagnosed by magnetic resonance cholangiopancreatography. He was admitted for ERCP.
ERCP was performed successfully over 0.035-inch diameter, 450-cm length straight-tip guide wire (Jagwire, Boston Scientific, Newton, USA). Pancreatic cannulation did not happen and after sphincterotomy, common bile duct stone was extracted with balloon easily. There was no visible bleeding on the course of the procedure. After ERCP the patient was followed for two hours and discharged after seeing normal values of amylase and hemogram. After six hours of ERCP the patient was admitted to emergency service with right upper quadrant pain, radiating to right shoulder and back and shortness of the breath. Blood pressure was 110/70 mmHg, pulse 86/min, body temperature 37.6°. He had compensated respiratory acidosis.
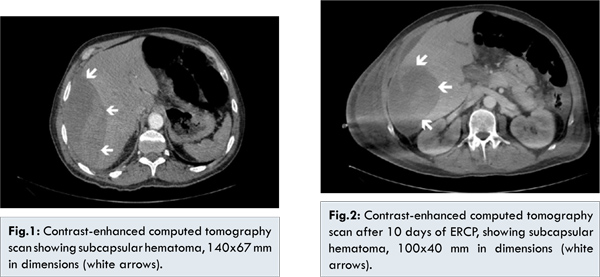
Laboratory tests revealed that serum total bilirubin of 1.9 mg/dL (normal less than 1.4 mg/dL) with conjugated bilirubin 0.5 mg/dL (normal less than 0.3 mg/dL), hemoglobin 16.1 g/dL (normal 13.3-17.7 g/dL), hematocrit 54% (normal 39-51%), aspartate aminotransferase 85 U/L (normal 0-40 U/L), alanine aminotransferase 134 U/L (normal 7-49 U/L), alkaline phosphatase 449 U/L, gamma glutamyltransferase 767 U/L (normal 10-71 U/L). Amylase and lipase were in normal range. Computerized tomography demonstrated that there was a 140x67 mm subcapsular hepatic hematoma in right lobe of the liver [Fig.1]. The patient was hemodynamically stable. He was hospitalized for further evaluation and treatment. Prophylactic antibiotics had been administered. During his follow-up the hematoma and hemodynamics of the patient was stable. However after 2 days of hospitalization, respiratory distress of the patient became worse and he was transferred to intensive care unit (ICU) for positive ventilation. He was followed in intensive care unit for 8 days and transferred to general surgery service again. A 10th day computed tomography revealed that hepatic hematoma regressed to 100x40 mm [Fig.2]. The patient gradually improved and was discharged from the hospital on 11th day. After 30 days of the ERCP the hematoma was completely resorbed.
ERCP is minimally invasive procedure for the diagnosis and treatment of biliary and pancreatic diseases. Complication rate is around 2.5% to 8% even in expert hands, with the mortality rate of 0.5% to 1% [
3,
4]. Clinically significant bleeding is seen in approximately 2% cases with the sphincterotomy. However endoscopically visible but non-detectable bleeding is about 10% to 30% with the sphincterotomy [
7]. Subcapsular hepatic hematoma after ERCP is rare complication that has been reported over 20 cases in the literature. It was firstly described by Ortega et al. [
5] in 2000 who diagnosed subcapsular hematoma in 81-year-old man with abdominal pain after ERCP for choledocholithiasis.
The etiology of the hematoma is not entirely clear. Most of the authors claim that it is caused by rupture of small caliber vessels due to the guide wire trauma [
8-
10]. Presence of air in the hematoma and growth of Citrobacter freundii from hematoma are supporting this idea [
5]. When we analyzed previously reported cases most patients were re-admitted to hospital with right upper quadrant pain. Our patient was also suffering from abdominal pain radiating to right shoulder and back. Patients are generally hemodynamically stable unless hematoma expands more. If the size of hematoma increases rapidly, hypotension, tachycardia and anemia may be seen [
8].
Management is mostly conservative as we did in our case. Glisson’s capsule of the liver keeps hematoma stable and prevents more bleeding. However large hematomas may require percutaneous drainage for symptomatic relief [
11]. We recommend broad spectrum antibiotics for these patients in the follow-up. Because guide wires used in ERCP are not sterile, so the hematoma may be infected. If the bleeding goes on and hematoma grows-up with the hemodynamic stability selective embolization can be done. It has been used in five cases in the literature, however two of them needed surgery thereafter [
3]. In our case hematoma did not grow up and hemodynamics of the patient was stable, so he did not require embolization and surgical treatment.
Surgical treatment is reserved for hemodynamic instability, infection or high risk of rupture. Surgical treatment should consist of adequate drainage of the hematoma and hemostasis of bleeding place. If re-bleeding occurs hepatic artery embolization should be kept in mind [
12].
Conclusion
Rare complication of hepatic hematoma after ERCP must keep in mind it if the patient complains of right upper quadrant pain or manifests hemodynamic instability. Recommended treatment is conservative follow-up by serial CT scans, percutaneous drainage. Hepatic artery embolization and surgery is inevitable in case of hemodynamic instability or increasing size of hematoma.
References
- Hart R, Classen M. Complications of diagnostic gastrointestinal endoscopy. Endoscopy.1990;22:229-233.
- Mallery JS, Baron TH, Dominitz JA, Goldstein JL, Hirota WK, Jacobson BC, et al. Complications of ERCP. Gastrointest Endosc. 2003;57:633-638.
- Zizzo M, Lanaia A, Barbieri I, Zaghi C, Bonilauri S. Subcapsular Hepatic Hematoma after Endoscopic Retrograde Cholangiopancreatography. A Case Report and Review of Literature. Medicine. 2015:94 (26):e1041.
- Hart R, Classen M. Complications of diagnostic gastrointestinal endoscopy. Endoscopy. 1990;22:229-233.
- Ortega Deballon P, FernándezLobato R, García Septiem J, Nieves Vázquez MA, Martínez Santos C, Moreno Azcoita M. Liver hematoma following endoscopic retrograde cholangiopancreatography (ERCP). Surg Endosc. 2000;14:767.
- Ertugrul I, Parlak E, Ibis M, Altiparmak E, Samaz N, Sahin B, et al. An unusual complication of endoscopic retrograde cholangiopancreatography. Dig Dis Sci. 2006;51:1167-1168.
- Freeman ML, Neslon DB, Sherman S, Haber GB, Herman ME, Dorsher PJ, et al. Complications of endoscopic biliary sphicterotomy. N Engl J Med. 1996;335:909-918.
- Klimova K, Suarez CP, Asanza CG, Pena AM, Arregui EG, Alonso AH. Subcapsular hepatic hematoma after ERCP: a case report and revision of literature. Sci Res. 2014;3:161-166.
- Cárdenas A, Crespo G, Balderramo D, Bordas JM, Sendino O, Llach J. Subcapsular liver hematoma after endoscopic retrograde cholangiopancreatography in a liver transplant recipient. Annals of Hepatology. 2008;7(4):386-388.
- Koçak E, Ergül B, Akbal E, Köklü S, Karakayali AS. Subcapsular hepatic hematoma after ERCP.Acta Gastroenterol Belg. 2012;75(1):63.
- Bhati CS, Inston N, Wigmore SJ. Subcapsular intrahepatic hematoma:an unusual complication of ERCP. Endoscopy. 2007;39Suppl 1: E150.
- Legaz JP, Santos J, Ruiz-Tovar J, Moya-Forcén P, Armañanzas L, Gómez M, Oller I, Arroyo A, Calpena R. Subcapsular hepatic hematoma after ERCP (endoscopic retrograde cholangipancreatography). Rev Esp Enfer Dig. 2011;103(10):550-551.