Introduction
Inflammatory myofibroblastic tumor (IMT) is a neoplasm of intermediate biologic potential [
1]. These tumors can involve many organs, with the urinary bladder being the most common site [
2]. Paratesticular inflammatory myofibroblastic tumor is a rare benign lesion that arises from testicular tunics and less commonly, grows into the epididymis and spermatic cord [
3]. They are often reported in the literature by various terms, e.g., proliferative funiculitis, inflammatory myofibroblastic tumor, pseudosarcomatous myofibroblastic proliferation and fibrous pseudotumor [
4]. This lesion is a consequence of a reactive proliferation of inflammatory and fibrous tissue [
3]. Currently, the term inflammatory myofibroblastic tumor has been generally accepted. The peak incidence is usually in the third decade of life but can occur at any age [
5].
Case Report
A 40 year old male presented to the surgical outpatient clinic with a painless scrotal swelling since 2 years and dragging sensation in groin area while walking. There was no previous surgical, traumatic or any other significant history. Physical examination revealed a firm, non-tender, and immobile mass in the right hemiscrotum measuring 4x3 cm with negative trans-illumination test. This mass was fixed to the inferior pole of the testis. Abdominal and inguinal examination failed to reveal mass or palpable lymph nodes. The left hemiscrotum was normal. Ultrasound examination showed a testicular mass underneath the inferior pole of testis. The mass was well circumscribed and heterogeneous, but globally hypoechoic relative to the testes. Due to unilateral scrotal swelling a possibility of testicular tumor was considered and serum markers for germ cell tumors (serum AFP, ß-HCG and LDH) were performed and were found within normal range. A provisional diagnosis of right testicular tumor was made and a right orchidectomy was done.
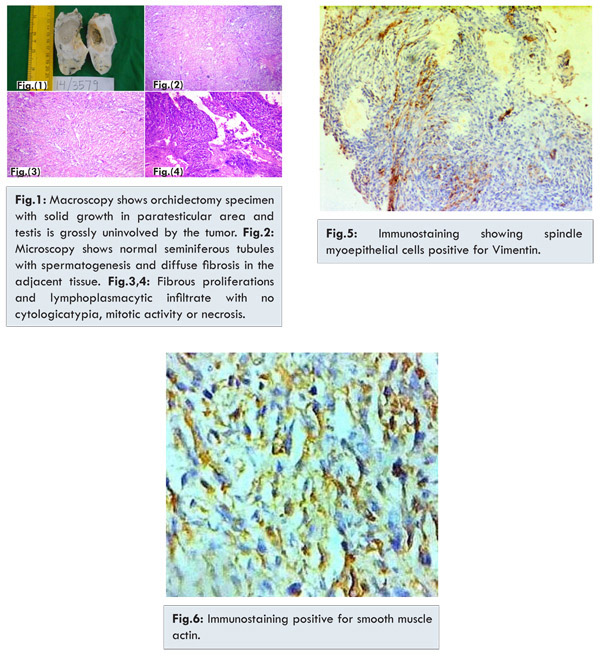
We received a right orchidectomy specimen with an area of ulceration measuring 3x2x1.5 cm on the outer aspect. Cut surface showed testis measuring 9.5x6x4.5 cm encased by thickened tunica and diffuse band like grey white growth. Testis was grossly uninvolved by the tumor. Microscopically, testicular tissue appeared normal with seminiferous tubules showing normal spermatogenesis covered with thickened tunica albuginea. Tumor was paratesticular with no connection with the testis and showed dense proliferation of spindle cells having abundant eosinophilic cytoplasm and plump elongated nuclei with bland chromatin. These areas were punctated by aggregates of chronic inflammatory cell infiltrate. No necrosis was noted however occasional mitotic figures were seen but none was atypical. Sections from ulcerated area of capsular rupture showed acute inflammatory exudate overlying spindle cell proliferation [Fig.1-6]. Thus a histopathological diagnosis of inflammatory myofibroblastic tumor was made.
Inflammatory myofibroblastic tumor (IMT) is an uncommon spindle tumor that may arise in multiple anatomic sites, including the lung, gastrointestinal tract, retroperitoneum, central nervous system, extremities, and the genitourinary tract. Although rare, paratesticular IMT represents the second most common paratesticular mass after adenomatoid tumor and comprises approximately 6% of such lesions [
6]. This term is generally accepted, though multiple names, such as inflammatory pseudotumor, proliferative funiculitis, chronic proliferative periorchitis, fibrous mesothelioma, and reactive periorchitis, are also assigned to this tumor. In 1904, Balloch first described fibrous pseudotumor involving the paratestis [5]. Most reported cases have involved the tunica vaginalis; rarely is it associated with the tunica albuginea, epididymis, or spermatic cord. The peak incidence of fibrous pseudotumors is in the third decade but can occur at any age [
3].
The etiology of IMT remains unclear. It is postulated that these lesions may represent an exaggerated reparative response to trauma, chronic irritation, or infection. Epstein-Barr virus, Mycobacterium avium-intracellulare, and human herpesvirus 8 have been cultured from pulmonary, splenic, and hepatic IMT; however, these infectious agents have not been identified in paratesticular IMT. Autoimmune etiology has also been suggested in tumors outside of the genitourinary tract [
6]. Tunica vaginalis is most commonly affected (75%), followed by epididymis (10%) and the remainder involving the spermatic cord or the tunica albuginea. Rarely paratesticular fibrous pseudotumors are associated with testicular infarction, Schistosomiasis, retroperitoneal fibrosis, Gorlin syndrome and HIV particularly the inflammatory variant [
5].
Paratesticular fibrous pseudotumors usually presents as unilateral painless mass mostly involving the left side [
8] ranging in size from 0.5 to 8 cm [
5]. The fibrous pseudotumors have non-specific appearances on ultrasonography. Diagnosis of the fibrous pseudotumor is difficult preoperatively due to non-specific features [
7] and may even be confused with testicular tumor or chronic testicular infarction. Macroscopically, these tumors present as ovoid nodules and occasionally encasing the testes as diffuse band-like fibrosis [
5] as in the present case. Microscopically, a variety of histologic patterns may be seen. They are composed of predominantly of cytologically bland spindle or stellate shaped cells loosely arranged in a myxoid stroma or hyaline with scattered inflammatory cells. Few of them are composed of a compact proliferation of spindle cells arranged in storiform or fascicular growth pattern. Small punctate areas of calcification, metaplastic bone, mitotic figures or lymphoplasmacytic infiltrate may be observed [
9]. Immunohistochemical staining will identify multiple fibroblasts, and is positive for Vimentin, smooth muscle-specific actin, and common muscle actin and negative for S-100, keratin, and desmin [
3].
More cellular cases of IMT should be distinguished from inflammatory leiomyosarcoma and even malignant lymphoma. Cigar shaped centrally located blunt nuclei are regarded as characteristic of leiomyosarcoma, but this is frequently obscured by infiltrating inflammatory cells especially in leiomyosarcoma, which leads to the misdiagnosis of inflammatory pseudotumors [
4]. Testicular sparing surgeries are not possible in most of the cases especially in cases of fibromatous periorchitis. Treatment of choice is scrotal exploration of the mass and frozen section biopsy [
8]. However, if testicular tumor cannot be excluded with certainty, radical orchidectomy is the procedure of choice [
6].
Conclusion
Fibrous pseudotumors are among the rarely seen benign tumors, and two-thirds involve the testicular tunica with rare involvement of other scrotal structures. These tumors may be confused with testicular tumors and should be always included in the differential diagnosis in young adults with testicular and paratesticular lesions.
References
- Rafeek N, Joseph LD, Rajendiran S, Narayanan CD. Inflammatory myofibroblastic tumor of spermatic cord. Int J Surg Case Rep. 2012;3(12):618-621.
- Kapur P, Treat K, Chuang ATY, Hoang MP. Pathologic Quiz Case: Paratesticular Mass in a Young Man. Arch Pathol Lab Med. 2004;128(5):589-590.
- Khallouk A, Ahallal Y, Tazi E, Tazi MF, Elfassi MJ, Farih MH. Benign Paratesticular Fibrous Pseudotumor With Malignant Clinical Features. Reviews in Urology. 2011;13(4):e203-e205.
- Kim NR, Gul Chung SYHJ, Han J. Inflammatory pseudotumor of the paratesticular area. Korean Journal of Pathology. 2004:38:208-211.
- Singh J, Hafiz A, Rasool M, Singh H, Sharma S, Bashir S. Fibrous pseudotumor of paratestis mimicking a testicular tumor. Open Pathology Journal. 2014.8.1-3.
- Harel M, Makari JH. Paratesticular inflammatory myofibroblastic tumor in a pediatric patient. Case Reports in Urology; Volume 2014 article 1D 303678.
- Ugras S, Yesil C. Fibrous pseudotumors of tunica albuginea, tunica vaginalis and epididymis: Report of two cases. Cancer Epidemiol. 2009;33:69-71.
- Tobias-machado M, Correa LNA, Heloisa SL, Borrelli M, Wroclawski ER. Fibrous pseudotumor of tunica vaginalis and epididymis. Urology. 2000;56(4):670-672.
- Goldblum John R, Folpe Andrew L, Weiss Sharon W. Borderline and malignant fibroblastic/myofibroblastic tumors. In: Enzinger & Weiss’s Soft Tissue Tumors. 6th edition. Elseviers Saunders:Philadelphia; 2014. pp.304-305.