Introduction
Hyperhomocysteinemia is a known risk factor for atherosclerosis, leading to venous and arterial thrombosis at an early age [
1]. It can involve different organ systems and manifest as stroke or ischemic heart disease or peripheral vascular disease [
2]. Hyperhomocysteinemia can be controlled by dietary supplements of vitamins B6 and B12 and folic acid, the cofactors in the metabolism of this amino acid [
2]. Here we report a young patient of hyperhomocysteinemia, who presented with superior mesenteric thrombosis and stroke at the same time. Our case is the first case of hyperhomocysteinemia simultaneously involving 2 different systems.
Case Report
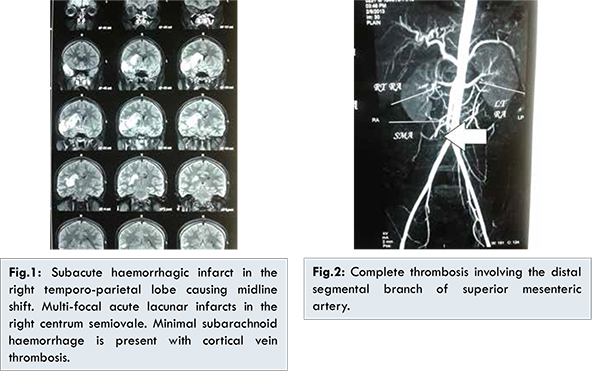
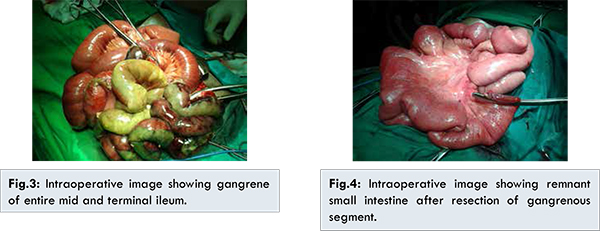
A 24 years old male presented with sudden onset of headache and left sided hemiparesis. He was a known alcoholic and nonsmoker. He had no history of diabetes mellitus, hypertension, hyperlipidemia or prior episode of vascular thrombosis. There was no known thrombotic disease in other family members. Magnetic resonance imaging of brain [Fig.1] showed subacute hemorrhagic infarct in the right temporo-parietal lobe causing mass effect and midline shift. Multifocal acute lacunar infarcts were seen in the right centrum semiovale. There was a minimal subarachnoid hemorrhage along the right fronto-parietal sulcal space with cortical vein thrombosis. Subsequently treatment was started in the line of management of stroke. After six hours of admission to hospital, he developed generalized abdominal distension with diffuse abdominal tenderness. Routine investigations showed elevated leucocyte count, neutrophilia, and mild elevated of serum creatinine. Contrast computerized tomography [Fig.2] of abdomen and pelvis showed complete thrombosis involving the distal segmental branch of superior mesenteric artery with signs of ischemic bowel of mid and terminal ileum and fluid in the abdomen. Patient underwent emergency laparotomy, which showed gangrene of entire mid and terminal ileum [Fig.3] with foul smelling hemorrhagic fluid in the abdomen. Resection of the gangrenous segment of the small intestine with proximal end ileostomy was performed [Fig.4].
A complete haemocoagulative profile comprising of protein C, protein S, antithrombin III, homocysteine, antiphospholipid antibodies and lupus anticoagulant, resistance to activated protein C, factors VII and VIII, mutation analysis of the prothrombin gene, and factor V Leiden was performed. All results were in the normal range except for the total homocysteine (HCY) level being high i.e. 174 µmol/L (normal value < 15 µmol/L). The levels of folic acid and cobalamin were low at 1 ng/mL (normal range 3-17 ng/mL) and 169 pg/mL (normal range 211-911 pg/mL), respectively. Lipid profile, ECG and cardiac echocardiography were normal. We did not check for methylene tetrahydrofolate reductase (MTHFR) gene mutations (both 677TT and 677CT) due to financial constraints. Post-operatively, the patient was put on anticoagulants, folate and vitamin B12 supplementation. He showed gradual improvement in motor and sensory functions in the left side of the body. On discharge his folate level improved and HCY levels decreased to 48 µmol/L. After 8 months, the side to side ileocolic anastomosis was performed to restore the bowel continuity. The patient is doing well after two years of follow up.
Discussion
Hyperhomocysteinemia is a metabolic disorder that results from abnormalities in the function of enzymes in the methionine metabolism pathway. It is a rare disorder with an incidence of the order of 1 in 2,00,000 to 10,00,000 population [
3]. This can be due to congenital defect or acquired deficiency of vitamins such as folate, vitamin B6 or B12 [
3]. Other less common causes of elevated HCY levels are advanced age, hypothyroidism, renal failure, lupus, leukemia, inflammatory bowel disease, liver disease, and certain drug such as oral contraceptives, theophylline, methotrexate, L-dopa, phenytoin, phenobarbital, and carbamazepine [
4]. Another hypothesis is that MTHFR gene mutations (both 677TT and 677CT) raise plasma levels of HCY, which produce an increased thrombotic risk for cardiovascular and cerebral vessels. Vitamin B12 is required as a cofactor for the enzyme MTHFR, which remethylates homocysteine to form methionine [
5]. Hence vitamin B12 deficiencies cause elevation HCY levels [
5].
Hyperhomocysteinemia results in angiopathies by involving a combination of endothelial cell oxidative damage, altered platelet activation, aggregation and vascular smooth muscle proliferation [
6]. It is suggested that HCY may promote thrombosis by enhanced tissue factor expression and factor V activity, suppression of thrombomodulin activity and decreased fibrinolysis [
7]. The other cause of elevated HCY level is low folate levels due to low dietary intake [
2]. Boushey et al. demonstrated a strong inverse relationship between HCY levels and plasma/dietary folate levels and decrease in HCY levels after administration of folic acid [
2]. In our case, his folate and vitamin B12 deficiency may be related to the alcoholism and associated malnutrition and HCY levels returned to normal after correction of folate and vitamin B12 during follow up.
Young patients below the age of thirty with severe hyperhomocysteinemia are at a high risk of a vascular event like myocardial infarction and stroke [
8]. Our case is first of its kind, where two different systems (gastrointestinal and neurological) are involved at the same time. All previous reports show either involvement of neuro or cardiac or other systems, involving only one system. This case highlights the importance of maintaining a high index of suspicion for any vascular thrombotic episodes in a young patient. In hyperhomocysteinemia, small doses of folic acid (1-5 mg/day) are generally efficacious. As additional therapy, low doses of pyridoxine, cyanocobalamin or choline usually normalize serum HCY levels in patients resistant to folate therapy [
9]. Dietary supplementation of folic acid, vitamins B6 and B12 effectively reduces the plasma level of homocysteine and, hence, may play a role in the prevention and therapy of atherosclerotic vascular disease [
10]. In our case chronic alcohol intake may also have contributed to vitamin deficiency. Abstinence from alcohol may be important to prevent nutritional deficiency in such cases.
Conclusion
Our case provides clinical evidence to support the association of hyperhomocysteinemia and vascular thrombosis. Young patients presenting with acute thrombosis of large vessels in the absence of an embolic source or atherosclerotic disease should be evaluated for abnormalities in HCY levels. A high index of suspicion and thorough evaluation are warranted to diagnose such rare cases.
References
- Verhoef P, Hennekens CH, Malinow MR, Kok FJ, Willet WC, Stampfer MJ. A prospective study of plasma homocyst(e)ine and risk of ischemic stroke. Stroke. 1994; 25(10):1924-1930.
- Boushey CJ, Beresford SA, Omenn GS, Motulsky AG. A quantitative assessment of plasma homocysteine as a risk factor for vascular disease: probable benefits of increasing folic acid intakes. JAMA. 1995;274(13):1049-1057.
- Yap S, Naughten ER, Wilcken B, Wilcken DE, Boers GH. Vascular complications of severe hyperhomocysteinemia in patients with homocystinuria due to cystathionine beta-synthase deficiency: effects of homocysteine lowering therapy. Semin Thromb Hemost. 2000; 26(3):335-340.
- Nourani Khojasteh H, Amiri A. Congenital lens dislocation and fatal cerebral vein thrombosis in a patient with homocysteinemia: A lesson for urgent screening of pediatric population. Arch Iran Med. 2013;16(5):306-307.
- Cattaneo M. Hyperhomocysteinemia and venous thromboembolism. Semin Thromb Hemost. 2006;32(7):716-723.
- Tan YM Chia KH. Acute Thrombosis Associated with Hyperhomocysteinemia. Eur J Vasc Endovasc Surg. 2002;24(3):279-280.
- Rees M. Homocysteinemia: association of a metabolic disorder with vascular disease and thrombosis. Thromb Res 1993;71(5):337-359.
- Graham IM, Daly LE, Refsum HM, et al. Plasma homocysteine as a risk factor for vascular disease: the European Concerted Action Project. JAMA. 1997; 277(22):1775-1781.
- Stabler SP, Marcell PD, Podell ER, Savage DG, Lindenbaum J. Elevation of total homocysteine in the serum of patients with cobalamin or folate deficiency detected by capillary gas chromatography-mass spectrometry. J Clin Invest. 1988;81(2):466-474.
- Zacarías-Castillo R, Hernández-Rebollar AE, Zajarias-Rabchinskey A, González-Bárcena D: Hyperhomocysteinemia. A new coronary risk factor. Gac Med Mex. 2001;137(4):335-345.