Introduction
The term posterior reversible encephalopathy syndrome (PRES) was first coined by Dr Judy Hinchey. She discovered this reversible phenomenon by assessing the Computed Tomography and Magnetic Resonance Imaging recordings showing white matter abnormalities without infarction in patients who mainly presented with headache, decreased alertness, altered mental functioning, seizures, and visual loss, including cortical blindness [
1]. Ever since term PRES has been coined, more and more cases are being categorized as PRES.
The causes are varied ranging from hypertensive encephalopathy, postpartum eclampsia, delayed postpartum preeclampsia and other hypertensive states which account for more than half of the cases [
2]. Other causes include renal diseases or immunosuppressive drugs for malignancy and transplantation. Though more cases of PRES are being reported it’s still considered a rare diagnosis. It is important to recognize it early and differentiate it from venous thrombosis or stroke which have completely different line of treatment and are usually suspected in such presentations. The delay in diagnosis and wrong management can cause additional complications and permanent neurological damage. We present here two cases of PRES.
Case Reports
Case 1
A 12 year old female presented to the emergency room of our hospital with three episodes of convulsions in the past three hours. The patient had been having headache, blurring of vision, vomiting since the past one day which were sudden in onset. There was progressive deterioration of symptoms in the next 24 hours. The patient had been diagnosed with hypertension six months back and was taking anti-hypertensives which were stopped four days back. On previous visit the patient had been advised for further investigations for the cause of hypertension but the patient had refused to get them done.
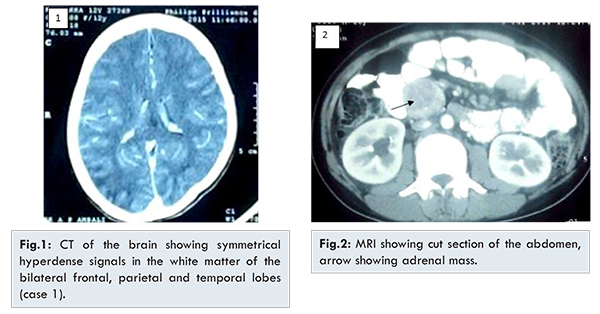
General physical examination was normal. Central nervous system examination revealed diminution of vision in both eyes with regard to perception of hand movement. Pupillary reactions were normal, a fundoscopic examination of eye showed early papilledema. Patient had normal power, tone and reflexes. Cardiovascular, respiratory and per abdomen examinations were normal. The patient was treated with a loading dose of phenytoin sodium and intravenous mannitol. She was started on prazosin 5 mg orally along with amlodipine 5 mg. The patients complete blood picture, liver function tests, kidney function tests, clotting parameters were within normal limits. Urine examination was normal. Echocardiogram showed global hypokinesia with features suggestive of myocarditis. The patient was diagnosed with hypertensive encephalopathy and imaging advised. CT brain showed symmetrical hyperdense signals in the white matter of the bilateral frontal, parietal and temporal lobes [Fig.1]. MRI of the abdomen showed adrenal mass [Fig.2]. Urine VMA levels were elevated to 22 mg/day.
The patient was diagnosed with posterior reversible encephalopathy syndrome secondary to pheochromocytoma. Regular blood pressure (BP) recordings were done. The mean BP was 190/100 mm of Hg. On fourth day the BP was 160/90 mm of Hg. Blood pressure returned to normal on the seventh day but the antihypertensives were continued. The patient underwent laparoscopic removal of the mass on the 14th day. Patient had complete resolution of symptoms and was discharged six days after surgery.
The patient returned for follow up after 1 month and had no residual symptoms. Repeat CT brain was done which showed complete disappearance of hyperdensities.
Case 2
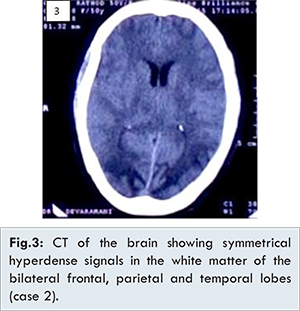
A 65 year old female presented to the emergency room with altered sensorium. She had one episode of loss of consciousness two hours back from which she had recovered in 15 minutes and has been in altered sensorium since then. The patient was not a known case of hypertension or cardiovascular disease. The blood pressure was recorded at 200/110 mm of Hg. On examination the patient was not oriented to time place or person with incoherent speech. Pupils were bilaterally reactive to light. Rest of the neurological examination was within normal limits. Other systems examination was normal. The patients complete blood picture, liver function tests, kidney function tests, clotting parameters were within normal limits. Urine examination was normal. The patient was diagnosed with hypertensive encephalopathy and imaging advised. CT brain showed symmetrical hyperdense signals in the white matter of the bilateral frontal, parietal, temporal lobes [Fig.3].
A diagnosis of PRES was made and the patient started on intravenous mannitol. A nitroglycerine infusion was started at 10 µg/kg body weight. As the blood pressure decreased to 160 mm Hg systolic, nitroglycerine was discontinued and oral amlodipine 10 mg three times a day was started. Blood pressure returned to normal on the third day, amlodipine was decreased to 10 mg once a day. Patient had complete resolution of symptoms and was discharged after six days.
The patient returned for follow up after 1 month and had no residual symptoms. Repeat CT brain was done which showed complete disappearance of hyperdensities.
Discussion
Advances made in imaging and increasing availability of CT and MRI in tertiary hospitals has made it possible to detect more cases of PRES. Cerebral edema, secondary to failure of cerebral autoregulation causing hyperperfusion has been widely cited as the possible pathophysiology of PRES. Another theory suggests ischemic damage secondary to vasoconstriction induced hypoperfusion which again causes cerebral edema [
3]. Vasogenic cerebral edema is easily picked up by CT and MRI which are very sensitive to changes in the distribution of water in the brain and make it possible to detect white-matter edema even in its early phases. Traditionally CT changes have been mainly reported to be seen in the posterior parietal-temporal-occipital regions of the brain but some studies show frontal lobe preponderance [
2].
Manifestations of PRES in the adult population include seizures, visual disturbances and headache. The other symptoms being nausea, vomiting, and blurring of vision [
4]. Studies have also revealed an altered autonomic response in patients with cyclical vomiting and there can be a heightened sympathetic cardiovascular tone and symptoms such as pallor, flushing, lethargy and fever [
5,
6]. The stress response may induce episodes of vomiting with infectious, physical or psychological stressors potentially triggering an episode [
7]. It has been reported that an increased level of adrenocorticotropic hormone (ACTH) and cortisol can be associated with lethargy and hypertension before the onset of vomiting [
8], and it has been hypothesized that corticotropin-releasing factor (CRF) may be a brain-gut mediator that directly connects stress and vomiting [
9].
Atypical cases include, cortical, brainstem lesions, hemorrhage into lesions, and unilaterality [
10]. Both our patients presented with signs of hypertensive encephalopathy on presentation. After imaging showed white matter hyperdensities and the patient’s symptoms started resolving with antihypertensives, PRES was considered as the diagnosis.
Conclusion
PRES is a rare disorder in children. Early recognition of characteristic radiological features is key to the diagnosis as clinical symptoms may be non-specific or mimic other neurological illnesses. This case emphasizes the need for early work up including imaging for cases who present with hypertension with end organ damage.
Acknowledgements
We would like to thank the departments of Radiology and Ophthalmology and for their contributions.
References
- Hinchey J, Chaves C, Appignani B, Breen J, Pao L, Wang A, et al. A reversible posterior leukoencephalopathy syndrome. N Engl J Med. 1996;334:494-500.
- Matthys LA, Coppage KH, Lambers DS, Barton JR, Sibai BM. Delayed postpartum preeclampsia: An experience of 151 cases. Am J Obstet Gynecol. 2004;190:1464-1466.
- Bartynski WS. Posterior reversible encephalopathy syndrome, part 2: Controversies surrounding pathophysiology of vasogenic edema. Am J Neuroradiol. 2008;29:1043-1049.
- Incecik F, Hergüner MO, Altunbasak S, Erbey F, Leblebisatan G. Evaluation of nine children with reversible posterior encephalopathy syndrome. Neurol India. 2009;57:475-478.
- Gordan N. Recurrent vomiting in childhood, especially of neurological origin.Dev Med Child Neurol. 1994;36:463-467.
- Fleisher DR. The cyclic vomiting syndrome described. J Pediatr Gastroenterol Nutr. 1995;21(Suppl 1):S1-5.
- To J, Issenman RM, Kamath MV. Evaluation of neurocardiac signals in pediatric patients with cyclic vomiting syndrome through power spectral analysis of heart rate variability. J Pediatr. 1999;135:363-366.
- Fleisher DR, Matar M. The cyclic vomiting syndrome: a report of 71 cases and literature review. J Pediatr Gastroenterol Nutr. 1993;17:361-369.
- Tache Y. Cyclic vomiting syndrome: the corticotropin-releasing-factor hypothesis. Dig Dis Sci. 1999;44:79S-86S.
- Kauntia R, Valsalan R, Seshadri S, Pandit VR, Prabhu MM. Late postpartum preeclampsia with posterior reversible encephalopathy syndrome. Indian J Med Sci. 2009;63:508-511.