claritin and pregnancy first trimester claritin pregnancy first trimester link
1Department of Tuberculosis and Respiratory Diseases, GSVM Medical College, Kanpur, Uttar Pradesh; 2Department of Pulmonary Medicine, U P Rural Institute of Medical Sciences & Research Saifai, Etwah, Uttar Pradesh; 3Department of Pulmonary Medicine, Maulana Azad Medical College, New Delhi.
Corresponding Author:
Dr. Prashant Yadav
Email: dr.prashantyadav10@gmail.com
Abstract
Echinococcosis or hydatid disease is caused by larvae of Echinococcus. The hydatid disease is endemic in some Mediterranean countries, Middle East, South America, South Africa and Oceania. The liver is the most common site of infection followed by the lung in 10% to 30% of cases. Pleural involvement of hydatid disease can occur, and usually follows the rupture of a pulmonary or hepatic hydatid cyst in to the pleural space. When a patient presents with recurrent pneumothorax, zoonotic infections, especially hydatid disease of the lung, should always be considered alongside other common causes of recurrent pneumothorax.
|
6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ffa4890d000000c704000001000800 6go6ckt5b5idvals|623 6go6ckt5b5|2000F757Tab_Articles|Fulltext Introduction
Echinococcosis or hydatid disease is caused by larvae of Echinococcus. In the life cycle of E. granulosus, humans sometimes become accidental intermediate hosts. The hydatid disease is endemic in some Mediterranean countries, Middle East, South America and South Africa and Oceania [ 1]. Hydatid disease is seen in any age and sex, although it is more common in those aged 20-40 years [ 2, 3]. Clinical symptoms depend on the location, number, and size of the cysts. The liver is the most common site of infection followed by the lung in 10% to 30% of cases, and other sites as spleen, kidney, brain, and in bone collectively about 10% cases. In lungs approximately 60% were located in the lower lobes, and a predilection for the right lung was seen in 56% cases [ 4]. Thoracic hydatidosis that are extrapulmonary are rare [ 5, 6]. Pleural involvement of hydatid disease can occur, and usually follows the rupture of a pulmonary or hepatic hydatid cyst into the pleural space. However, primary pleural involvement by a slowly enlarging cyst is very rare. Here in this case of recurrent pneumothorax, pleural hydatid cyst infestation was diagnosed as a cause of recurrent pneumothorax.
Case Report
A 24 years old male presented with shortness of breath, dry cough and left sided chest pain for two months. There was history of left intercostal drainage of chest 6 months back at district hospital and the chest tube was removed after 10 days. There was no history of any chronic illness like diabetes mellitus, hypertension, asthma, contact with tuberculosis, blood transfusion, weight loss or illicit drug intake. On examination, he was afebrile, conscious, and oriented. His pulse rate was 110/min, respiratory rate was 30/min, blood pressure 130/80 mm Hg and oxygen saturation was 90% on room air. There was no pallor, jaundice, oedema, clubbing or lymphadenopathy. He was thin built with body mass index of 18.75 kg/m2.
Respiratory system examination revealed the trachea was shifted to the right, the apex beat was felt in the right hemithorax, decreased movement on left side of hemithorax, decreased vocal fremitus on left side of chest. The left chest was hyper-resonant on percussion with diminished vocal resonance and on auscultation respiratory breath sounds were absent and heart sounds were audible in the right chest. Abdominal examination, cardiovascular and nervous examinations were within normal limits.
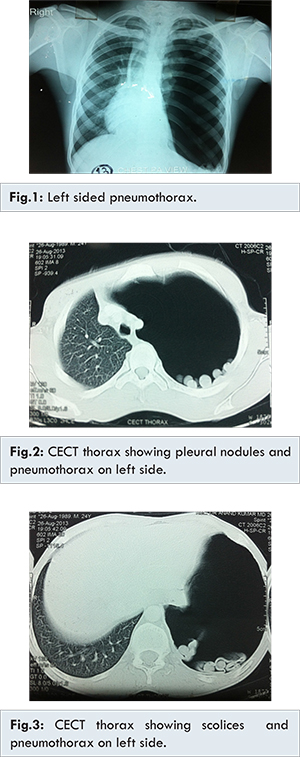
Laboratory investigation showed haemoglobin 11 g/dL, white blood cells count 13000/mm3 (polymorph 89%, lymphocytes 11%) and platelets 2.5 lacks/mm3. His liver function and renal function tests were normal and hepatitis B surface antigen, VDRL and HIV antibodies were negative. ECG showed no abnormalities. Sputum for acid fast bacilli (AFB) was negative for AFB. A chest radiograph showed large left-sided pneumothorax with shift of the upper and lower mediastinum towards the opposite side [Fig.1] and multiple small (around 2 cm) nodular shadows on left hemithorax. The chest computed tomography scan revealed a large left side pneumothorax and complete collapse of left lung and multiple pleural nodules and scolices of Taenia [Fig.2,3]. Abdominal sonography showed only mild fatty liver without any cysts or masses in the liver. Hydatid serology (echinococcus IgG ) was positive (85.34 U/mL).
Pneumothorax was treated by immediate needle decompression followed by tube thoracostomy [Fig.4] and intercostal drainage was removed after 10 days. Albendazole 400 mg twice in a day was given for 6 weeks. The patient made an unremarkable recovery and discharged after 3 weeks. On long-term follow-up, the patient remained healthy and there was no recurrence.
Discussion
Hydatid cysts form in the liver in 50% to 79% of patients and in the lung in 10%-30%. They may also be found in the muscles, bones, kidneys, brain, heart, and other organs. Most cysts are acquired in childhood, remain asymptomatic for a long period of time, and are later diagnosed incidentally at chest radiography. Pulmonary hydatid cysts are multiple in 30% of cases, bilateral in 20%, and located in the lower lobes, mostly right, in 60% [ 7, 8]. Of patients with lung cysts, liver cysts are seen in 20%-40% [ 9, 10]. Within the chest, echinococcosis can primarily involve the pleural cavity [ 11]. Thoracic hydatidosis that are extrapulmonary are rare [ 4, 5]. The clinical features of cystic hydatidosis are variable, depending on the size, number of cysts and their location in the thorax, their interaction with the surrounding organs. Chronic cough, shortness of breath and chest pain is seen in patients with cysts in the pleural cavity, because of the compression of the trachea-bronchial tree and lung volume reduction. Mediastinal cysts may cause compression of the major vessels and trachea. They may present with complications like rupture and spread of protoscolices and larval material into pleural cavity or blood vessels, bacterial infection of cysts. Rupture of the pulmonary hydatid cyst is not very uncommon complication. Rupture can occur either into the pleural cavity or bronchus [ 12]. Rupture into pleural cavity present as pleural effusion and subsequent complications include infection leading to empyema in 7.6% cases, pleural thickening, collapsed lung, simple pneumothorax in 2%-6% cases [ 13] and tension pneumothorax [ 12], Immunologic reactions such as asthma, anaphylaxis, or membranous nephropathy secondary to release of antigenic material are not uncommon. Hydatid cysts are encountered in the intact or ruptured form. Cyst rupture might be seen spontaneously or as a result of trauma When a hydatid cyst ruptures, it is termed as a complicated cyst and patient presentation is quite variable depending on the nature of the perforation [ 14].
The most important diagnostic tools in pulmonary hydatid cysts are plain X-ray and CT scan [ 15]. CT scan has been reported to be the most sensitive diagnostic tool [ 16]. It is typical for an intact cyst to present as a round or oval homogenous density with sharp contours [ 15]. The current gold standard serology test for echinococcosis detects IgG antibodies to hydatid cyst fluid-derive native or recombinant antigen B subunits. This is performed using ELISA or immunoblot formats [ 17]. ELISA test with crude hydatid cyst fluid has a high sensitivity of 95%; however, its specificity is low at 61% [ 18]. Echinococcus granulosus has a very complex antigenic structure, and hydatid disease has a slowly developing course. From 3% to 40% of human hydatidosis cases, most of which involve the lung, are found to be seronegative [ 19]. In our case multiple rounded shadows in chest X-ray [Fig.1] made us suspect an echinococcal etiology for recurrent pneumthorax. The combination of imaging and serology established the diagnosis in our case.
Conclusion
This case report suggests that when a patient presents with recurrent pneumothorax, zoonotic infections, especially hydatid disease of the lung, should always be considered alongside other common causes of recurrent pneumothorax.
References
- Gharbi HA, Hassine W, Brauner MW, Dupuch K. Ultrasound examination of the hydatic lover. Radiology. 1981;139:459-463.
- Dogan R, Yuksel M, Cetin G, Suzer K, Alp M, Kaya S, et al. Surgical treatment of hydatid cysts of the lung: report on 1055 patients. Thorax. 1989;44:192-199.
- Zapatero J, Madrigal L, Lago J, Baschwitz B, Perez E, Candelas J. Surgical treatment of thoracic hydatidosis. A review of 100 cases. Eur J Cardiothorac Surg. 1989;3:436-440.
- Jerray M, Benzart M, Garrouche A, Klabi N, Hayouni A. Hydatid disease of the lungs: study of 386 cases. Am Rev Respir Dis. 1992;146:185-189.
- Ozvaran MK, Ersoy Y, Uskul B, Unver E, Yalcin E, Baran R, et al. Pleural complications of pulmonary hydatid disease. Respirology. 2004;9:115-119.
- Kabiri el-H, Caidi M, al Aziz S, el Maslout A, Benosman A. Surgical treatment of hydatidothorax. Series of 79 cases. Acta Chir Belg. 2003;103:401-404.
- Morar R, Feldman C. Pulmonary echinococcosis. Eur Respir J. 2003;21:1069-1077.
- Pedrosa I, Saiz A, Arrazola J, Ferreiros J, Pedrosa CS. Hydatid disease: radiologic and pathologic features and complications. Radiographics. 2000;20:795-817.
- Gomez R, Moreno E, Loinaz C, De la Calle A, Castellon C, Manzanera M, et al. Diaphragmatic or transdiaphragmatic thoracic involvement in hepatic hydatid disease: surgical trends and classification. World J Surg. 1995;19:714-719.
- Dogan R, Yuksel M, Cetin G, Süzer K, Alp M, Kaya S, et al. Surgical treatment of hydatid cysts of the lung: report on 1055 patients. Thorax. 1989;44:192-199.
- Aribas OK, Kanat F, Gormus N, Turk E. Pleural complications of hydatid disease. J Thorac Cardiovasc Surg. 2002;123:492-497.
- Balci AE, Eren N, Eren S, Ulka R. Ruptured hydatid cysts of the lung in children: clinical review and results of surgery. Annals of Thoracic Surgery. 2002;74(3):889-892.
- Aribas OK, Kanat F, Gormus N, Turk E. Pleural complications of hydatid disease. Journal of Thoracic and Cardiovascular Surgery. 2002;123(3):492-497.
- Kuzucu A, Soysal O, Ozgel M, Yologlu S. Complicated hydatid cysts of the lung: clinical and therapeutic issues. Ann Thorac Surg. 2004;77:1200-1204.
- Sahin E, Enon S, Cangir AK, Kutlay H, Kavukcu S, Akay H, et al. Single-stage transthoracic approach for right lung and liver hydatid disease. J Thorac Cardiovasc Surg. 2003;126:769-773.
- Gulalp B, Koseoglu Z, Toprak N, Satar S., Sebe A, Gökel Y, et al. Ruptured hydatid cyst following minimal trauma and few signs on presentation. Netherlands Journal of Medicine. 2007;65(3):117-118.
- Craig PS, McManus DP, Lightowlers MW, Chabalgoity JA, Garcia HH, Gavidia CM, et al. Prevention and control of cystic echinococcosis. Lancet. 2007;7:395-394.
- Ammann RW, Eckert J. Cestodes: echinococcus. Gastroenterol Clin North Am. 1996;25:655-689.
- Gadea I, Ayala G, Diago MT, Cunat A, de Lomas JG. Immunological diagnosis of human cystic echinococcosis: utility of discriminant analysis applied to the enzyme-linked immunoelectrotransfer blot. Clin Diagn Lab Immunol.1999;6:504-508.
|