Introduction
The four layered fatty sheet of peritoneum is known as omentum and suspends from the greater gastric curvature to surrounding organs with attachments to the diaphragm [
1]. Torsion of the greater omentum can be either primary or secondary. Primary torsion of the greater omentum, first reported by Eitel in 1899, occurs when the omentum twists upon itself, with the formation of a narrow neck in the absence of associated intra-abdominal pathology [
2]. It mainly affects adults, with men being involved twice as frequently as women, with the majority being overweight [
3]. Omental torsion is rarely diagnosed preoperatively and may lead to spontaneous clinical deterioration of the patient [
4]. We report a case of primary omental torsion in a middle age man diagnosed on CT scan.
Case Report
A 42 old male patient presented to the Emergency Department complaining of generalized abdominal pain for one week, localizing to the right mid and lower abdomen. Associated vomiting, nausea and constipation were main complaints. Abdominal examination revealed tenderness and guarding especially in the right side of abdomen with diminished abdomen sounds. McBurney sign was positive but all the other appendicular signs were negative. Lungs were clean to auscultation and the cardiocirculatory examination was negative. No urinary symptoms, past medical history of note or regular medication were present. Laboratory tests noticed leukocytosis and raised CRP. An ultrasound scan showed, diffuse probe tenderness in right mid and lower abdomen with raised mesenteric echogenicity. Signs of appendicitis were negative on ultrasound. Due to inconclusive ultrasound, patient subsequently underwent CT study.
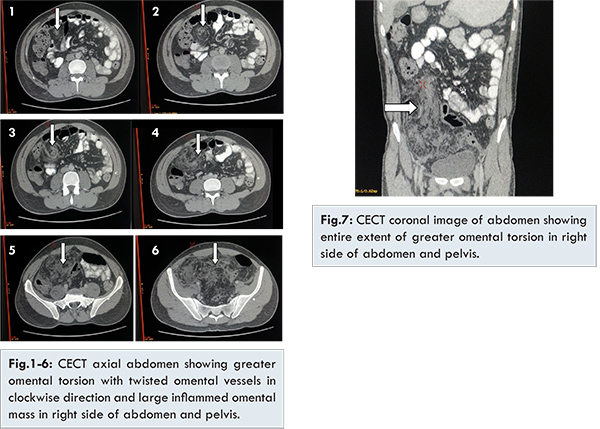
An abdominal computed tomography (CT) scan [Fig.1-6] revealed twisting of the greater omentum with typical whirlpool appearance of twisted omental vessels in right mid-abdomen and large inflamed omental fatty mass extending upto right lower abdomen as well as pelvic cavity displacing bowel loops along its margins. No evidence of ascites or bowel dilatation was seen. Coronal reconstructed CT [Fig.7] revealed entire extent of greater omentum in right side of abdomen extending into pelvic cavity.
On laparotomy large inflammatory omental mass consisting of a section of infarcted omentum and twisted omental vessels were identified. Intraoperatively [Fig.8,9] inflamed greater omental mass with at least three twists and no associated bowel obstruction or abnormal dilatation found. No obvious adhesions were seen surrounding the omental torsion. The small bowel was normal and intact. The infarcted omentum was resected [Fig.10]. Resected gross specimen of omentum was showing areas of necrosis and hemorrhage with diffuse inflammation.
Discussion
Omental torsion is a rare cause of abdominal pain presenting mainly in the 3rd to 5th decade of life with a slight male predominance (3:2) [
5,
6]. The omentum twists around its long axis, clockwise at a pivotal point. Consequently vascularity is compromised, resulting in hemorrhagic extravasation, serosanguinous fluid production, necrosis and adhesion formation.
Omental torsion is of two types. In primary torsion, anatomic malformations such as bifid or accessory omentum causes a spontaneous torsion; sudden movements and hyper-peristalsis have been implicated as precipitating factors. Obesity is also a well-documented risk linked to primary torsion, with one study documenting that almost 70% of patients with omental infarction were obese [
7]. It is postulated that excess fat unevenly distributed in the omentum acts as a lead point for torsion. Secondary torsion occurs most often because of hernia, tumor, or adhesion, with the dependent omentum becoming fixed in the torsed position and unable to untwist. Both of these processes may lead to infarction of the affected omentum [
8]. Secondary torsion is more common and a result of underlying abdominal pathology (e.g. cysts, adhesions, hernial sacs) resulting in a distal fixation point [
9]. Our patient seems to have had none of these predisposing or precipitating conditions mentioned.
The primary symptom associated with omental torsion is pain, which is frequently localized in the right lower quadrant of the abdomen. The onset of pain is usually sudden and does not radiate to the abdominal wall [
10]. In many cases, the pain localizes in the right lower quadrant and reveals signs of peritoneal irritation. Bowel movements are usually normal, and nausea and vomiting are rare. Differential diagnosis should include appendicitis, cholecystitis, caecal diverticulitis, perforated duodenal ulcer, abdominal wall hematoma, and intestinal obstruction [
11]. In women of reproductive age and children’s differential diagnosis like salpingitis, ovarian cyst torsion, ectopic pregnancy, Meckel diverticulum and mesenteric adenitis [
5] are included.
Imaging investigations such as ultrasonography and Computed Tomography (CT) have been suggested in the literature [
12]. On sonography a complex mass consisting of hypoechoic and solid zones may be identified, but this imaging technique is operator dependent with limited sensitivity due to overlying bowel gas [
13]. CT scan is considered the examination of choice in cases of acute abdomen. A basic advantage of CT versus sonography is the reliability of identifying the mass in the characteristic location between the anterior abdominal wall and the colon [
14]. Specific CT findings in omental torsion include diffuse inflamed omental mass with whirling pattern fatty folds and vessels [
15]. In our case, though, CT demonstrates the twisted omental part but ultrasound scan was not specific. Specific CT findings in our case were clockwise twisted omental vessels in right anterior abdomen with large inflamed fatty omental mass extending from right mid abdomen to the pelvic cavity and displacing bowel loops peripherally. No associated abnormal bowel dilatation, obstruction, adhesion or mass lesions were seen. Patient subsequently underwent laparotomy and intra-operative findings were similar to that of CT imaging features [
16]. In our case, intraoperatively large fatty omental mass found in the right side of abdomen with torsion of omental vessels and areas of hemorrhage as well as necrosis. Clockwise twisting of omental mass was found with no bowel adhesion or intestinal obstruction. No signs of bowel herniation or any abnormal mass lesion found in the abdomen.
Conclusion
Omental torsion is rare condition and differential diagnosis of the acute abdomen especially with acute appendicitis. CT scan is investigation of choice in suspected case of omental torsion; it can accurately demonstrate the omental torsion and rule out other causes of acute abdomen. Appropriate management of omental torsion should be the surgical. Intraoperative findings have good correlation with preoperative CT imaging features.
References
- Theriot JA, Sayat J, Franco S, Buchino JJ. Childhood obesity: a risk factor for omental torsion. Pediatrics. 2003;112 (6 Pt 1): e460-10.1542/peds.112.6.e460.G. G.
- Eitel. Rare omental torsion. NY Med Rec. 1899;55:715-716.
- Mavridis G, Livaditi E, Baltogiannis N, Vasiliadou E, Christopoulos G. Primary omental torsion in children: ten-year experience. Pediatric Surgery International. 2007;23(9):879-882.
- Parr NJ, Crosbie RB. Intermittent omental torsion--an unusual cause of recurrent abdominal pain? Postgraduate Medical Journal. 1989;65:114-115.
- Tsironis A, Zikos N, Bali C, Pappas-Gogos G, Koulas S, Katsamakis N. Primary Torsion of the Greater Omentum: Report of Two Cases and Review of the Literature. The Internet Journal of Surgery. 2008;17(2):16.
- Al-Jaberi T, Gharaibeh K, Yaghan R. Torsion of abdominal appendages presenting with acute abdominal pain. Annals of Saudi Medicine. 2000;20(3-4):211.
- Van Breda Vriesman AC, Lohle PNM, Coerkamp EG, Puylaert JBCM. Infarction of omentum and epiploic appendage: diagnosis, epidemiology and natural history. European Radiology. 1999;9:1886-1892.
- Itenberg E, Mariadason J, Khersonsky J, Wallack M. Modern management of omental torsion and omental infarction: a surgeon’s perspective. Journal of Surgical Education. 2010;67(1):44-47.
- Saber A, LaRaja R. Omental Torsion. E Medicine, article 191817. 2007, Available from: http://emedicine.medscape.com. Accessed on June 29, 2016.
- Maeda T, Mori H, Cyujo M, Kikuchi N, Hori Y, Takaki H. CT and MR findings of torsion of greater omentum. Abdominal Imaging. 1997;22(1):45-46.
- Naffaa LN, Shabb NS, Haddad MC. CT findings of omental torsion and infarction: case report and review of the literature. Clinical Imaging. 2003;27(2):116-118.
- Abdennasser el K, Driss B, Abdellatif D, Mehci A, Souad C, Mohamed B. Omental torsion and infarction: CT appearance. Intern Med. 2008;47(1):73-74.
- Schlesinger AE, Dorfman SR, Braverman RM. Sonographic appearance of omental infarction in children. Pediatric Radiology. 1999;29(8):598-601.
- Grattan-Smith JD, Blews DE, Brand T. Omental infarction in pediatric patients: sonographic and CT findings. The American Journal of Roentgenology. 2002;178:1537-1539.
- Abdennasser EK, Driss B, Abdellatif D, Mehci A, Souad C, Mohamed B. Omental torsion and infarction: CT appearance. Internal Medicine. 2008;47:73-74.
- Aoun N, Haddad-Zebouni S, Slaba S, Noun R, Ghossain M. Left-sided omental torsion: CT appearance. European Radiology. 2001;11(1):96-98.