Tugba Özbek1, Nesibe Kahraman Çetin1, Nilgün Kuman Kanlioglu2, Serdar Sen2, Ibrahim Halil Erdogdu1, Ibrahim Meteoglu1
Department of Pathology1 and Thoracic Surgery2, Adnan Menderes University, Medical School, Aydin, 09100, Turkey.
Corresponding Author:
Dr. Ibrahim Meteoglu
Email: imeteoglu@hotmail.com
Abstract
The result of dismigration during organogenesis, thyroid gland can rarely present outside their usual anatomical localization, especially midline cervical, thoracic and abdominal cavity. The lung is a rare localization for ectopic thyroid tissue. Most patients are asymptomatic. However, they can be noticeable as a solitary pulmonary nodule, during tests conducted for other purposes, or during autopsy. A 47-year-old female patient presented with chest pain for 3 months. She had a past history of subtotal thyroidectomy for nodular goitre 31 years ago. Computed tomography showed anterobazal segment nodule in right lower lobe of lung. After thoracotomy, dirty yellow, solid nodular lesion, 1 cm in diameter, was observed in lung wedge resection material. Histological examination showed the lesion was separated with a sharp boundaries from the lung parenchyma, had non-teratogenic components, and thyroid tissue was found with a colloid-containing follicular structures. Immunohistochemical staining showed TTF-1 and thyroglobulin expression in this area. With these findings the patient was diagnosed as ectopic thyroid tissue. We want to emphasize that although it is rare, ectopic thyroid tissue can be localized intrapulmonary, and this should be considered in the differential diagnosis of pulmonary nodules.
|
6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ff64640e000000d904000001001b00 6go6ckt5b5idvals|635 6go6ckt5b5|2000F757Tab_Articles|Fulltext Introduction
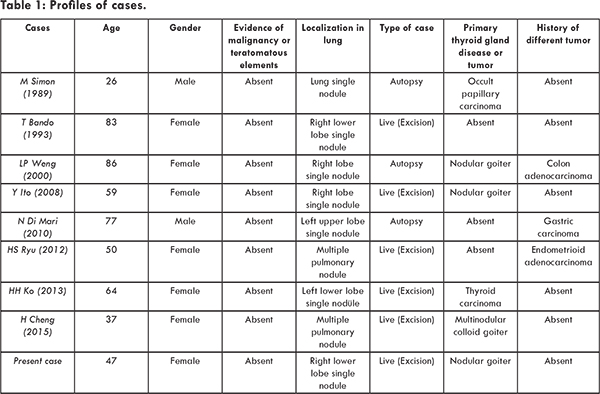
Heterotopic thyroid tissue is the presence of thyroid tissue at any sites along its embryologic path other than the usual thyroid position in the neck. It is a rare developmental anomaly [1,2]. Although ectopic thyroid tissue is rare, with a reported incidence of 1 in 300,000, it is most frequently reported between the foramen caecum and the normal position of the thyroid gland, often in the base of the tongue, as a lingual thyroid [1,3]. The other common sites for an ectopic thyroid gland are thyroglossal duct, the coupling between the foramen cecum and thyroid gland, and laryngotracheal region [1]. It is rare, but there have been reports of ectopic tissue in the lung, submandibular region, the trachea, the mediastinum, the heart, the duodenum, the adrenal gland, the parotid gland and the gall bladder [3]. Intrapulmonary heterotopic thyroid is a rare form of ectopic thyroid tissue with only eight cases reported so far [4-11]. As in our case, the nodules were always single [4-10]. Only two case of bilateral intrapulmonary ectopic thyroid has been reported [9,11] [Table 1].
A 47 year old female presented to the hospital with a history of chest pain for last 3 months. She had a past history of subtotal thyroidectomy for nodular goiter 31 years ago and was subsequently followed by medical treatment. In the computed tomography, captured there, solitary nodule was detected in the segment of the right lower lobe in anterobasal, and patient was referred to our hospital [Fig.1]. The patient, underwent thoracotomy and pulmonary wedge resection was carried out.
In macroscopic evaluation of wedge resected specimen of lung, 5.5 cm, dirty yellow specimen with 1 cm in diameter, solid, nodular lesion was observed. On microscopic examination of the lesion, thyroid tissue that had colloid content and follicular structures lined with monomorphic cells was seen [Fig.2]. It was well-defined, had non-teratogenic components and separated by sharp boundaries from the usual lung parenchyma. Around the lesion there was mild chronic inflammation in a restricted area. The lung parenchyma outside this area was normally observed. The lesion was stained positive with the immunohistochemical TTF-1 and thyroglobulin [Fig.3]. With all these findings the patient was diagnosed as intrapulmonary ectopic thyroid tissue.
Discussion
The presence of thyroid tissue anywhere along its embryologic path other than the usual thyroid position in the neck is defined as heterotopic thyroid tissue [1,2]. It is a rare developmental anomaly. The prevalence of thyroid ectopia is higher in females than in males [12]. The lung is a quite rare localization for ectopic thyroid tissue and location of heterotopic thyroid tissue in the lung parenchyma is difficult to explain on basis of embryology. One possibility is that during early embryologic life, there may be abnormal contact of the thyroid and the respiratory diverticulae, both of which originate from the primitive foregut endoderm and are anatomically close to each other. This may result in implantation of thyroid cells in the respiratory diverticulum and eventually in the lungs. The second possibility is metaplasia of lung cells into thyroid cells given that both organs share a common embryologic origin from the foregut endoderm [10]. Most cases of ectopic intrapulmonary thyroid are asymptomatic and it is incidently detected as a solitary pulmonary nodule or noticeable during autopsy [5]. Sometimes it can cause symptoms with mass effect such as dysphagia, dysphonia, stidor, dyspnea, hemorrhage, and hoarseness [12]. Ectopic thyroid may become goitrogen and may also be associated with clinically evident thyroid dysfunction, which could be either hypofunction or hyperfunction. Rarely, benign or malignant neoplastic changes can occur. Thyroiditis occurring in ectopic thyroid tissue has also been reported. Hyperthyroidism arising from ectopic thyroid tissue is less common than hypothyroidism. However, an ectopic thyroid gland with histological features of Graves’ disease has been found in different locations like the base of the tongue, mediastinum, submandibular region, lateral neck and the mesentry of the small intestine [13]. Thyroid tissue was sharply separated from the lung parenchyma as histologically and thin, connectival septa incompletely separated it into distinct lobular units. Follicles had a normal, benign appearance with a cuboidal epithelium and abundant fluid colloid. It doesn’t contain teratomatous components and it has a positive immunohistochemical staining seen with thyroglobulin [8].
A differential diagnosis of ectopic intrapulmonary thyroid includes thyroid cancer metastasis, thymoma, neuroma, germ cell tumor and all kinds of metastatic tumors. Ectopic thyroid may progress to malignant papillary thyroid carcinoma. Prior to ectopic intrapulmonary thyroid treatment, the patient’s age, presence of orthotropic thyroid, symptoms due to nodules and their severity, thyroid hormone level and malignancy potential need to be considered to perform surgical or medical treatment. Depending on the position of the tissue, sternotomy or thoracotomy can be performed for surgical treatment. Also, thoracoscopic treatment can also be considered.
In conclusion, ectopic thyroid tissue is rare and elusive diagnosis that is usually asymptomatic, but can be symptomatic depending on its location, size, and risk of malignancy. Surgical treatment can be performed considering the presence of symptoms or malignancy [10]. One must maintain a high degree of suspiction in any patient presenting with intrapulmonary nodules.
References
- Lianos G, Bali C, Tatsis V, Anastasiadi Z, Lianou E, Papathanasiou V, Meddinis T. Ectopic thyroid carcinoma. G Chir. 2013;34(4):114-116.
- Abujrad H, Olberg B, Ooi TC. Heterotropic Pulmonary Thyroid in the Presence of a Normally Located Multinodular Goitre. J Clin Case Rep. 2012;2(7):134.
- Bertha A, Julie Hephzibah, Nylla Shanthly. Ectopic thyroid - a case series. Journal of Clinical and Diagnostic Research. 2011;5(2):291-293.
- Simon M, Baczako K. Thyroid inclusion in the lung. Metastasis of an occult papillary carcinoma or ectopia? Pathol Res Pract. 1989;184:263-267.
- Bando T, Genka K, Ishikawa K, Kuniyoshi M, Kuda T. Ectopic intrapulmonary thyroid. Chest. 1993;103:1278-1279.
- Weng LP, Kaiser A, Koch HH, Wünsch PH. Multilocular thyroid gland ectopy. Dtsch Med Wochenschr. 2000;125:421-424.
- Ito Y, Yabuta T, Hirokawa M, Fukushima M, Inoue H, Uruno T. Distant and lymph node metastases of thyroid nodules with no pathological evidence of malignancy a limitation of pathological examination. Endocr J. 2008;55:889-894.
- Di Mari N, Barbagli L, Mourmouras V, Miraco C. Case report-Ectopic thyroid of the lung. An additional case. J Pathologica. 2010;102(3):102-103.
- Ryu HS, Chung YJ, Chong S, Lee JL, Ectopic intapulmonary thyroid tissue mimicking metastatic tissue. Thyroid. 2012;22:755-759.
- Ko HH, Cho SW, Lee HS, Kim HS, Nam ES, Cho SJ. Ectopic Intrapulmonary Thyroid: A Case Report. Korean J Thorac Cardiovasc Surg. 2013;46(3):237-239.
- Cheng H, Yang L, Xiong J, Peng J, Ruan Q. Multipl thyroid nodules in the lung: metastasis or ectopia? Diagnostic Pathology. 2015;10.1:1-6.
- Amanda K. Heterotopic Thyroid. Journal of Diagnostic Medical Sonography. 2004;20 (2):120-123.
- Nasiru AI, Idowu OF. Ectopic thyroid: etiology, pathology and management. Hormones. 2011;10(4):261-269.
|