Introduction
Cavernous hemangiomas of the uterus are extremely rare, benign lesions. A survey of the literature identified fewer than 50 cases of hemangioma of the uterus. Although they can be found at all levels of the uterine wall, including the serosa, myometrium and endometrium, most cases usually involve the myometrium diffusely. These lesions are associated with numerous obstetric and gynecological complications, ranging from inter-menstrual spotting, meno-metrorrhagia and infertility to maternal and fetal demise from pronounced bleeding of the gravid uterus [
1-
4]. We present a rare case of a cavernous hemangioma in a 42 years non-pregnant woman with a history of heavy menstrual bleeding refractory to medical management.
Case Report
Mrs.A, 42 year-old female, presented with a three-year history of polymenorrhagia. Three years back, her cycles were of 28-30 days duration with bleeding of 3-4 days, but for last 3 years, her menstrual cycle length was decreased to 15-20 days and with heavy flow lasting for 8-10 days for which she uses 4-5 pads/day. It was associated with passage of clots and mild pain in lower abdomen. She is P2L2 with last child birth 14 years back. Both her deliveries were lower segment caesarean section done for cephalopelvic disproportion. In the past, she had been using IUCD as a method of contraception but it was spontaneously expelled in after two years of insertion.
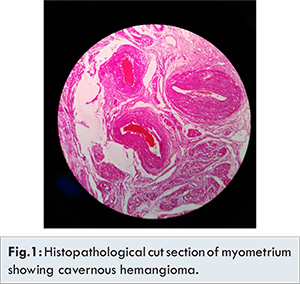
She came to gynecological OPD for these symptoms. On examination, she was found to be anaemic, bleeding was present coming through os, and uterus was regularly enlarged, about 12 weeks of gravid uterus size. On ultrasonography, utero-cervical length was 14 cm with cystic spaces in myometrium, suggestive of adenomyosis uterus. She was advised intravenous iron (ferric-carboxy maltose) for correction of anemia. Further, she was advised endometrial biopsy along endocervical curettage. The histopathology report showed endometrial hyperplasia along with polyp and negative for any intraepithelial malignancy. Thereafter progesterone containing intrauterine contraceptive device was placed as a part of medical management which resulted in relief of her symptoms. But the device was spontaneously expelled after four months. Then injection DMPA was given but no improvement was shown by the patient. So in view of failed medical management total laproscopic hysterectomy with bilateral salpingectomy was done in September 2015 and the specimen was sent for histo-pathological examination. Histopathological examination shows cavernous hemangioma of uterus with deep type adenomyosis along with endometriosis of bilateral fallopian tube.
A cavernous hemangioma of the uterus may either occur as an isolated lesion of the uterus [
4-
9] or may be associated with pelvic or extra-pelvic hemangiomatosis [
10]. There have been few case reports that describe isolated involvement of the uterus in pregnant women and highlight the importance of uterine cavernous hemangioma as a rare but important cause of refractory uterine bleeding at the time of delivery [
4,
5]. Uncommonly, they may be localized to a portion of the uterus and present in a non-pregnant woman with either uncontrolled vaginal bleeding [
4-
6], menorrhagia (as in our case), or unremitting pelvic pain. Recent literature documents only three published cases of cavernous hemangioma in non-pregnant women. In two cases, the women were peri-menopausal. In the third case, a 14-year-old female had to undergo an emergent hysterectomy for life-threatening bleeding [
5]. All the cases of endometrial hemangiomas described in the literature have shown progressive symptoms of uterine bleeding non-responsive to conservative therapy [
1-
3]. Most of these lesions are asymptomatic and incidental diagnosis, but sometimes they may cause abnormal uterine bleeding and hence should be included in the differential diagnosis of patients with uterine bleeding. With this condition, investigations such as vaginal examination, endometrial curettage, ultrasound, and hysterogram are non-informative and inconclusive. In a few cases the uterus has been reported to be pulsatile [
4]. If there is any clinical suspicion in cases not responding to conservative treatment, a pelvic angiogram and CT may confirm the presence of a lesion.
Based on a review of the literature and our own findings, it can be suggested that a cavernous hemangioma has no predilection for age and that its relationship to pregnancy is coincidental. It can further be theorized that localized forms of a cavernous hemangioma preexist and mainly go undetected during pregnancy or delivery. Uterine bleeding and/or unremitting pelvic pain associated with a localized cavernous hemangioma are generally unresponsive to current treatment options. In pregnant women, close follow-up is recommended as it can increase the rate of successful vaginal and Cesarean section deliveries with retention of the uterus [
4,
5]. In non-pregnant women, uterine artery embolization or internal artery ligation is conservatively recommended; however, the exact choice remains debated. In any patient not responding to conservative treatment, the possibility of a hysterectomy should be discussed
The present case highlights clinical symptom of unremitting menorrhagia in a non-pregnant female refractory to medical management, 14 years after the last uneventful delivery with concomitant presence of an adenomyotic foci. Since, these cases can present with an uneventful obstetric history, the clinical suspicion needs to be high as an early diagnosis and intervention can decrease future complications.
Conclusion
A localized cavernous hemangioma of the uterus is a rare lesion that may be clinically silent during pregnancy and may present with menorrhagia or unrelenting pelvic pain.
References
- Malhotra S, Sehgal A, Nijhawan R. Cavernous hemangioma of the uterus. Int J Gynaecol Obstet. 1995;51(2):159-160.
- Dawood MY, Teoh ES, Ratnam SS. Ruptured haemangioma of a gravid uterus. J Obstet Gynaecol Br Commonw. 1972;79(5):474-475.
- Johnson C, Reid-Nicholson M, Deligdisch L, Grinblat S, Natarajan S. Capillary hemangioma of the endometrium: a case report and review of the literature. Arch Pathol Lab Med. 2005;129(10):1326-1329.
- Benjamin MA, Yaakub HR, Telesinghe P, Kafeel G. A rare case of abnormal uterine bleeding caused by cavernous hemangioma: a case report. J Med Case Reports. 2010;4:136.
- Virk RK, Zhong J, Lu D. Diffuse cavernous hemangioma of the uterus in a pregnant woman: Report of a rare case and review of literature. Arch Gynecol Obstet. 2009;279:603-605.
- Sharma JB, Chanana C, Gupta SD, Kumar S, Roy K, Malhotra N. Cavernous hemangiomatous polyp: An unusual case of perimenopausal bleeding. Arch Gynecol Obstet. 2006;274:206-208.
- Uzunlar AK, Yilmaz F, Kilinç N, Arslan A. Cavernous hemangioma of the uterus: A case report. Eur J Gynaecol Oncol. 2002;23:72-73.
- Malhotra S, Sehgal A, Nijhawan R. Cavernous hemangioma of the uterus. Int J Gynaecol Obstet. 1995;51:159-160.
- Salm R. Diffuse cavernous haemangioma of the uterus. J Pathol Bacteriol. 1959;77:111-115.
- Djunic I, Elezovic I, Ljubic A, Markovic O, Tomin D, Tadic J. Diffuse cavernous hemangioma of the left leg, vulva, uterus, and placenta of a pregnant woman. Int J Gynaecol Obstet. 2009;107:250-251.