Introduction
Congenital broncho-esophageal fistula being diagnosed in adults is very rare. Majority of these cases are associated with esophageal atresia, hence symptoms occur immediately after birth. Rarely few patients may remain symptom free for years or may have minimal symptoms to get diagnosed in later life. Less than 300 cases in adults have been reported in world literature [
1].
Case Report
A 31 year old female patient presented with history of cough with expectoration since last three months. Cough was insidious in onset and immediately after swallowing food. Sputum was purulent and contained food particles. These symptoms were accompanied by intermittent fever since seven days prior to hospitalization. She had no history of breathlessness, chest pain, hemoptysis, halitosis, regurgitation of food dysphagia and upper gastrointestinal symptoms. No past history of similar symptoms, corrosive poisoning, contact with tuberculosis, foreign body inhalation, surgery, addiction or neurological symptoms could be elicited.
Her symptoms were typical of aspiration on food intake. Common causes for aspiration in an adult are lower cranial nerve palsy, acquired anatomical abnormalities due to trauma and obstruction due to neoplasm/stricture/stenosis. This patient did not give any history suggestive of any of these causes. On examination she was conscious, alert, oriented. Higher mental functions were normal. She was moderately built and nourished. General physical examination was unremarkable. Respiratory rate was 22/minute, afebrile. She had fine crepitation’s in left infra scapular area. No other systemic abnormality was detected.
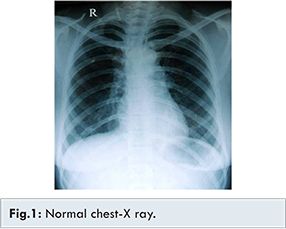
Blood routine examination showed raised total count with neutrophilia. Sputum smear for acid fast bacillus was negative. Sputum culture grew Klebsiella pneumoniae. Chest X-ray was normal [Fig.1]. Since her symptoms were typical of aspiration, provisional diagnosis of trachea-esophageal fistula was made. To prevent further aspiration Ryle’s tube feeding was started. She was started on broad spectrum antibiotics.
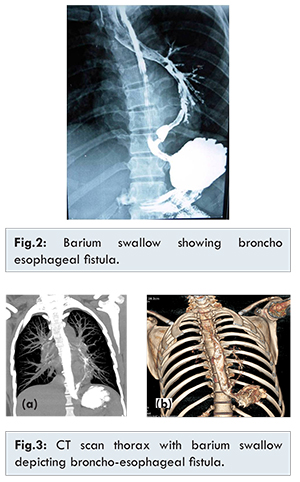
The investigation of choice in a suspected trachea-esophageal fistula is barium swallow. Hence barium swallow was done. Barium swallow showed broncho-esophageal fistula. Fistulous tract was seen connecting lower 3rd of esophagus to left lower lobe bronchus with retrograde filling of left main bronchus and trachea [Fig.2]. Upper gastro-intestinalscopy showed a small opening around 3 cm above the gastro-esophageal junction. Mucosa around the opening was normal. CT scan thorax with barium swallow was done. It showed reflux of barium into the anterior segment bronchus of left lower lobe from distal esophagus through a fistulous communication at the esophageal hiatus level. There was minimal patchy opacity in left lower lobe [Fig.3]. Bronchoscopy showed bronchial end of the fistula in the left lower lobe bronchus with no signs of inflammation. A final diagnosis of congenital broncho-esophageal fistula was confirmed as investigations did not reveal any cause for acquired fistula.
Treatment of choice for congenital broncho-esophageal fistula is surgery. Thoracotomy showed the fistulous tract starting from 3 cm above the gastro-esophageal junction running obliquely upwards to enter the left lower lobe anterior segment at the base of the lung [Fig.4]. The lung was healthy. No inflammation or adhesions were seen. Hence a simple fistulectomy was done. Esophageal stump was closed with diaphragmatic buttress. Pulmonary end was transfixed with pleural buttress. She made uneventful complete recovery after surgery.
Histopathology showed fistula tract lined by stratified squamous epithelium with underlying fibromuscular stroma. Lympho-plasmocytic infiltration was seen indicating chronic inflammation. There was no evidence of dysplasia or malignancy [Fig.5]. Hence benign fistulous tract was confirmed.
Discussion
Fistulous communication between tracheo-bronchial tree and esophagus due to common embryological origin is not uncommon. Most often the communication occurs between trachea and esophagus. Congenital broncho-esophageal fistula is rare as most often the communication occurs between trachea and esophagus. Most cases manifest immediately after birth as they are associated with esophageal atresia [
1]. Persistence of congenital fistula manifesting in adults for the first time is a very rare condition. Less than 300 cases in adults have been reported in world literature.
In an adult broncho-esophageal fistula is most often acquired. Most common cause is esophageal carcinoma eroding into a bronchus. Rarely bronchogenic carcinoma can also involve the esophagus. Other causes for acquired bronchoesophageal fistula include: (i) trauma (ii) infection (tuberculosis, fungal) (iii) radiation. Broncho-esophageal fistula is almost three times more common on the right side than the left and the most frequent site of communication is the right lower lobe [
2]. The criteria for diagnosing a congenital broncho-esophageal fistula by histopathology of resected fistulous tract include [
3]: (i) absence of inflammation and lymphadenitis, (ii) presence of mucosa, (iii) muscularis mucosa and transition of the lining epithelium from squamous to columnar. Histopathology of resected fistulous tract in our case fulfilled all these criteria. Majority of patients with bronchoesophageal fistula have cough on swallowing liquids (Ono’s sign) or food in the sputum [
4]. Conventional barium swallow is the most sensitive means for the diagnosis of broncho-esophageal fistula [
5-
7].
Following may be the reasons for delayed manifestation of broncho-esophageal fistula with symptoms appearing for the first time in adults. There may an occlusive membrane that ruptures later in life to open the fistulous tract [
8]. A mucosal fold may act as a valve and may lose its occlusive effectiveness after chronic inflammation [
9]. Obliquity of the fistulous tract may permit its closure during swallowing [
10]. The fistula, which is always invested with a smooth muscle coat, has the ability to contract, thus narrowing or completely occluding its lumen which may open in later life [
11]. We postulate that if the esophageal end of the fistula is at a lower level as in our case patient may remain asymptomatic as significant aspiration may not occur because of gravity. Treatment of choice is surgery. Fistulectomy with simple closure of the openings in both ends is done [
12]. In some cases the lung becomes repeatedly infected and lung resection may be required if underlying lung is diseased [
12]. Prognosis is excellent in patients who undergo surgical repair [
13].
Majority of patients with broncho-esophageal fistula develop severe aspiration pneumonia which may be fatal if not recognised and treated promptly. Our patient did not show significant lung lesion despite having symptoms for three months. This may due to the fact that the esophageal end of the fistula was at a much lower level and the tract was oblique. Hence probably due to gravity she had less aspiration and maybe there was back drain into the esophagus which prevented infection and inflammation in the lung.
References
- Maeta H, Toyota N, Ikeda M, Honboh T, Iwanaga Y. Congenital and acquired esophagobronchial fistula. Kyobu Geka. 2006;59:215-220.
- Juhani RO, Salo JA, Mattila SP. Congenital bronchoesophageal fistula in the adult. Ann Thorac Surg. 1995;59:887-890.
- Smith DC. A congenital broncho-oesophageal fistula presenting in adult life without pulmonary infection. Br J Surg. 1970;57:398-400.
- Brainbridge MV, Keith HI. Esophagobronchial fistula in the adult. Thorax. 1965;20:226-233.
- Rämö OJ, Salo JA, Mattila SP. Congenital bronchoesophageal fistula in the adult. Ann Thorac Surg. 1995;59:887-889; discussion 890.
- Lazopoulos G, Kotoulas C, Lioulias A. Congenital bronchoesophageal fistula in the adult. Eur J Cardiothorac Surg. 1999;16:667-669.
- Aguiló R, Minguella J, Jimeno J, Puig S, Galeras JA, Gayete A, Sánchez-Ortega JM. Congenital bronchoesophageal fistula in an adult woman. J Thorac Cardiovasc Surg. 2006;131:916-917.
- Jackson C, Coates GM. The nose, throat and ear andtheir diseases. Philadelphia: Saunders, 1929:1124.
- Mullard KS. Congenital tracheooesophageal fistula without atresia of the oesophagus. J Thorac Surg. 1954;28:39-54.
- Demong CV, Grow JB, Heitzman GC. Congenital tracheoesophageal fistula without atresia of the oesophagus. Am Surg. 1959;25:156-162.
- Osinowo O, Harley HRS, Janigan D. Congenital broncho-oesophageal fistula in the adult. Thorax. 1983;38:138-142.
- Joo Hyun Kim, Kay-Hyun Park, Sook Whan Sung, Joon Ryang Rho. Congenital Bronchoesophageal Fistulas in Adult Patients. Ann Thorac Surg. 1995;60:151-155.
- Ramo OJ, Salo JA, Mattila SP. Congenital bronchoesphageal fistula in the adult. Ann Thorac Surg. 1995;59:887-889.