6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ffa817200000002307000001000400
6go6ckt5b5idvals|832
6go6ckt5b5|2000F757Tab_Articles|Fulltext
Introduction
Mediastinal emphysema refers to presence of air within the mediastinum while subcutaneous emphysema refers to the presence of air in the subcutaneous tissue involving face, neck or trunk [
1]. The term pneumo-mediastinum was introduced into medical literature by Hamman in 1939 [
2]. Both the conditions are uncommon, but important complications of bronchial asthma. First such case was reported in a child in 1850, though Laennec in 1819 had recognized signs and symptoms of subcutaneous emphysema [
3]. We are presenting a case of pneumo-mediastinum and subcutaneous emphysema complicating an acute exacerbation of asthma in a young female to sensitize treating physicians of this unexpected complication. González García L. et al reported a case of non-invasive ventilation (NIV) complicating a similar case warranting mechanical intubation in the patient [
4]. Considering this as an uncommon presentation, it is imperative for emergency physicians to have a high degree of suspicion in such cases.
Case Report
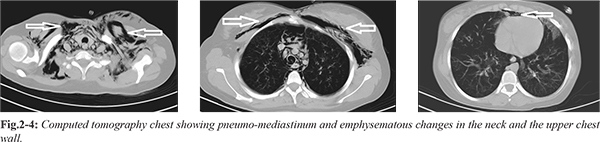
A 20 year old female complaining of cough and dyspnea since five days presented to the Emergency Department (ED) at an urban tertiary care hospital. She also had a complaint of neck pain and swelling since one day. Patient was unmarried, non-smoker and was a known case of bronchial asthma since childhood. She had a history of non-compliance to medications. She was administered nebulised medication one day prior at another health centre facility. On admission her pulse rate was 140/min, respiratory rate: 24/min and blood pressure: 110/70 mmHg. She was saturating at 89% on room air which increased to 98% on 6-7 L/min humidified oxygen by face mask. Chest auscultation revealed extensive bilateral rhonchi. On further examination patient had palpable crepitations in supra-clavicular fossa extending to neck bilaterally. Auscultation on neck revealed rhonchi with crepitations on pressure. Chest X-ray showed normal lung fields with increased lucency along subcutaneous tissue of neck and axilla bilaterally diagnostic of subcutaneous emphysema in neck region and bilateral axilla [Fig.1]. She further underwent high resolution computed tomography chest which revealed significant pneumo-mediastinum and marked emphysematous changes noted in the soft tissues of visualised neck and the upper chest walls [Fig.2-4]. On the basis of the history, examination and radiological findings, a diagnosis of acute exacerbation of bronchial asthma with pneumo-mediastinum and subcutaneous emphysema was made. She was treated with nebulized salbutamol and parenteral hydrocortisone. She was further admitted into the intensive care unit under the pulmonology team where she was kept on oxygen enriched air, bronchodilators, parental antibiotics and steroids, oral oseltamivir and other supportive treatment. Patient gradually improved and finally patient left the hospital against medical advice.

Discussion
Subcutaneous emphysema is a rare complication of acute severe asthma that may occur in association with spontaneous pneumo-mediastinum, pneumo-pericardium or pneumo-peritoneum. Spontaneous pneumo-mediastinum arises as a result of sudden rise in intra-alveolar pressure (asthma, vasalva manouvre, cough, emesis, barotraumas) resulting in the rupture of marginal alveoli and subsequent tracking of air along bronchi, interstitial and vascular support tissues into the mediastinum. The itinerant molecules of air may get to the pleural, pericardial, peritoneal space or the soft tissues of the face, neck or upper trunk causing subcutaneous cervico-facial emphysema. Other causes of extravasations of air into extra-pulmonary structures include rapid ascent to the water surface after diving, dental extraction, adenoid-tonsillectomies, trombone playing, bowel perforation, paraquat intoxication, arthroscopy and strangulation of the neck from hanging [
5-
7].
In this case, there were clinical and radiological evidence for the subcutaneous emphysema. Management of this condition is largely conservative. However, administration of high concentration of oxygen may enhance faster absorption of air from extra-pulmonary tissues while needle aspiration and/ or surgical decompression may be useful if mediastinal structures are compressed [
8].
Extra-pulmonary extravasations of air manifesting as pneumo-mediastinum and subcutaneous emphysema is a rare but important complication of acute exacerbation of bronchial asthma. Administration of positive pressure ventilation via NIV can lead to further increase in the above mentioned complications [
4].
Conclusion
Discharging patients or escalating patients unresponsive to standard therapies on invasive and NIV management without ruling out the same can have disastrous outcomes. Thus, we would like to emphasize that the emergency physicians require a high index of suspicion to diagnose this rare complication in patients presenting as acute exacerbation of bronchial asthma.
Contributors: AV: manuscript writing, literature review, patient management; SA, WRS: manuscript editing, literature review, and patient management. MH, SJ: critical inputs into the manuscript and patient management. WRS will act as guarantor. Both authors approved the final version of this manuscript.
Funding: None; Competing interests: None stated.
References
- Maunder RJ, Pierson DJ, Hudson LD. Subcutaneous and mediastinal emphysema: pathophysiology, diagnosis and management. Arch Intern Med. 1984;144:1447-1453.
- Hamman L. Spontaneous mediastinal emphysema. Bull John Hopkins Hosp. 1939;64:1-21.
- Mcgovern JP, Ozkaragoz K, Roett K, Haywood TH, Hensel Jnr AE. Mediastinal and subcutaneous emphysema complicating atopic asthma in infants and children; review of the literature and report of occurrence in an infant two years of age. Paediatrics. 1961;27:951-960.
- González García L, Rey C, Medina A, Mayordomo-Colunga J. Severe subcutaneous emphysema and pneumomediastinum secondary to non-invasive ventilation support in status asthmaticus. Indian Journal of Critical Care Medicine. 2016;20:242-244.
- Inna K, Bartolome RC. Pneumomediastinum in a 63 year old woman with asthma exacerbation. Chest. 2000;117:1778-1881.
- Shackelfold D, Casani JA. Diffuse subcutaneous emphysema, pneumomediastinum and pneumothorax after dental extraction. Ann Emerg Med. 1993;22:248-250.
- Aghayev E, Yen K, Sonnenschein M, Jackowski C, Thali M, Vock P, et al. Pneumomediastinum and soft tissue emphysema of the neck in postmortem CT and MRI; a new vital sign in hanging? Forensic Sci. Int. 2005;153:181-188.
- Newcomb AE, Clarke CP. Spontaneous pneumomediastinum: A benign curiosity of a significant problem? Chest. 2005;128:3298-3302.