6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ffe436200000006607000001000500
6go6ckt5b5idvals|836
6go6ckt5b5|2000F757Tab_Articles|Fulltext
Introduction
Tuberculosis is known to affect almost every organ in the body [
1]. Tuberculosis of head and neck area, excluding laryngeal tuberculosis is relatively uncommon. It constitutes only 2-6% of extra-pulmonary tuberculosis and 0.1-1% of all forms of tuberculosis [
2,
3]. Retro-pharyngeal abscess is a rare presentation, even in the presence of extensive pulmonary tuberculosis [
4,
5]. However, in recent years, there has been a surge in incidences of extra-pulmonary tuberculosis. Here we report an unusual case of tuberculous retro-pharyngeal abscess presenting as dysphagia in middle aged male, without any past history of pulmonary tuberculosis.
Case Report
A 51 year old known chronic smoker male presented to our hospital with complaints of progressive oropharyngeal dysphagia since 14 days. The patient described that a solid food bolus could not be propelled successfully after swallowing and used to regurgitate through the nose, whereas liquid swallowing sometimes caused coughing. The initial diagnosis by his general practitioner was reflux disease. His symptoms did not improve after the administration of proton pump inhibitors, so he was referred to our hospital. The patient also had complaints of on and off fever since 14 days along with severe neck pain and hoarseness of voice. The patient did not mention any other symptoms.
His general examination revealed a swelling in the neck region with cervical lymphadenopathy. It was associated with restriction of neck movements. There was no skin thickening, discoloration or features suggestive of any connective tissue disorders and other systems were unremarkable. Central nervous system examination was suggestive of impaired sensation over the posterior one-third of the tongue, palate, and pharynx; and an absent gag reflex. Physical examination performed in the ENT department was also unremarkable. The patient was apyrexic at presentation and did not mention any night sweating. Flexible endoscopy of the vocal cords, auscultation of the lungs was normal.
Laboratory investigations revealed white blood cell, 5000/µL (neutrophils, 63.9%; lymphocytes, 28.6%); hemoglobin: 13.2 g/dL; hematocrit 39.5; and erythrocyte sedimentation rate, 40 mm/hour. C-reactive protein was 2 mg/dL. Hepatitis B surface antigen and antibodies for HIV and hepatitis C virus were negative. The chest x-ray was normal. Tuberculin (Mantoux) test was positive. In view of neck rigidity lumbar puncture was done which revealed TLC-5 cell/mm3, all lymphocytes; sugar: 63 mg%; protein: 43 mg%; Gram staining and AFB were negative.
Ultrasonography of the neck was done, which was suggestive of a para-pharyngeal abscess. A CT scan of the neck was performed, which revealed a para-vertebral abscess causing compression over hypo-pharynx and upper part of esophagus. The para-vertebral abscess extended into neural foramina of C3-4 and C4-5 and causing compression of exiting nerve routes. The patient was empirically started on anti- tubercular therapy, the patient received isoniazid (300 mg), rifampicin (600 mg), pyrazinamide (1500 mg), and ethambutol (1200 mg) for 2 months, followed by isoniazid (300 mg) and rifampicin (600 mg) for 4 months. A neuro-surgical opinion was sought for possible intervention however was deferred at attendant’s refusal. The patient made an uneventful recovery with complete remission of the lesion.
Discussion
The retro-pharyngeal area is a potential space in between the bucco-pharyngeal facia and the pre-vertebral facia. The contents include pre-vertebral lymph nodes (in children) and areola tissue. The former forms part of the lymphatic drainage of the head and neck region, which may explain why retro-pharyngeal abscess is common in children [
6]. Acute retro-pharyngeal abscess is, therefore, uncommon in older children and adults, except as a consequence of trauma to the head and neck region [
7]. Chronic retro-pharyngeal abscess seen in adults, is usually caused by a tuberculous infection of the cervical spine as pus spreads directly through the anterior longitudinal ligament [
8]. Alternatively, it may be due to tuberculous process involving the retro-pharyngeal lymph nodes [
9]. Retro-pharyngeal tuberculous abscess is a rare presentation of tuberculosis, even in patients with extensive pulmonary disease. The continuation of the retro-pharyngeal space in the superior and posterior mediastinum explains its importance for the spread of infection to the chest [
10].
In our patient, there were no classical symptoms of spinal tuberculosis and thus the diagnosis was delayed. The classic symptoms of patients with retro-pharyngeal abscess are dysphagia, odynophagia, and airway obstruction. In more severe cases, external neck swelling or neck rigidity may be present. Sometimes, hoarseness and stridor may also develop either due to anterior displacement of the posterior pharyngeal wall by the abscess or secondary laryngeal edema [
11]. The propensity of cervical lesions to cause neurologic deficit may explained by the fact that the spinal canal in this region is small relative to the diameter of the cervical cord. The classic symptoms of tuberculosis such as weight loss, night sweats, and cachexia may not be seen always [
12]. Patients with tuberculosis of the spine (Pott disease) present with restricted movements of the neck and pain at the back of the neck. Local inflammatory response, tuberculous vasculitis and ischemia, sub-luxation of the vertebrae, abscess on the spinal cord or nerve root, and impingement of the discs are the mechanisms responsible for neurological symptoms. As the abscess expands, it may bulge anteriorly into the airway and cause respiratory obstruction, or it may compress the spinal cord and cause weakness of the extremities [
8]. The diagnosis is based on a high index of clinical suspicion, especially in an endemic area, a positive tuberculin (Mantoux) test, radiologic features, aspiration of the mass for bacteriologic examination and culture, biopsy for histo-pathologic examination, enzyme-linked immunosorbent assay, and polymerase chain reaction [
7].
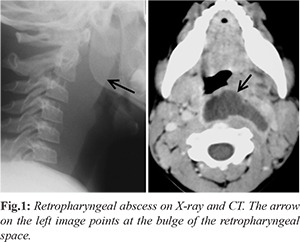
A lateral soft tissue radiograph of the neck on inspiration can provide a simple and useful aid to the diagnosis. Suspicion should be raised when there is narrowing of the disc space, loss of paradisc space, kyphotic deformity, and soft tissue shadow [
11]. Ultrasonography can provide a simple, cheap, and non-irradiating investigation, but a negative result cannot rule out a deep abscess in the neck [
10]. Computed tomographic scan can define the abscess dimensions, location, and possible extensions but has limitations in distinguishing cellulitis from an abscess and can lead to false-positive results. Magnetic resonance imaging scanning can diagnose any complications more accurately, such as vein thrombosis [
7]. Extra-pulmonary tuberculosis is common among HIV-infected patients; therefore, all patients should be screened for the disease [
12].
According to the findings of the Medical Research Council prospective study on TB spine, overall outcome was similar for both conservative (medical) and operative treatments. The report, however, advocated that patients with neurologic deficits, unstable spine, kyphosis, abscess, and intractable pain require surgery. The patient in our case was managed on conservative treatment, and showed complete recovery from the lesion.
Conclusion
The diagnosis of tuberculous retro-pharyngeal abscess is based on careful patient's history and examination along with a high index of clinical suspicion. Delay in diagnosis and treatment can lead to complications such as spontaneous rupture of the abscess leading to tracheo-bronchial aspiration, or stridor due to laryngeal oedema, or mediastinitis. Fever, neck pain and dysphagia should elicit the clinical suspicion of tubercular abscess in the retropharyngeal space.
Contributors: AKM: manuscript editing, patient management; RA, KKG: manuscript writing, patient management; RS: critical inputs into the manuscript and patient management. AKM will act as guarantor. All authors approved the final version of this manuscript.
Funding: None; Competing interests: None stated.
References
- Christoforidou A, Metallidis S, Kollaras P, Agathangelidis A, Nikolaidis P, Vital V, Markou K. Tuberculous retropharyngeal abscess as a cause of oropharyngeal dysphagia. Am J Otolaryngol. 2012;33:272-274.
- Alvarez S, McCabe W. Extrapulmonary tubrerculosis revisited: a review of experience at Boston City & other hospitals. Medicine (Balt). 1984;63:25-55.
- Weir M, Thosnton G. Extrapulmonary tuberculosis. Am J Med. 1985;79:467-476.
- Melchor Diaz MA, Domingo Carrasco C, Monge Jodra R, Marino Espuelas J, Ontanon Martin M. Tuberculous retropharyngeal abscess in an HIV patient: Report of a case. Acta Otorhinolaryngol Esp.1993;44:467-470.
- Thomas MD, Tierney PA, Samuel D, Patel KS. Tuberculosis: an unusual cause of dysphagia. Otolaryngol Head Neck Surg. 1995;113:644-650.
- Tannebaum RD. Adult retropharyngeal abscess: a case report and review of the literature. J Emerg Med. 1996;14:147-158.
- Meher R, Agarwal S, Singh I. Tuberculous retropharyngeal abscess in an HIV patient. Hong Kong Med J. 2006;12:483-485.
- Kamath MP, Bhojwani KM, Kamath SU, Mahabala C, Agarwal S. Tuberculous retro-pharyngeal abscess. Ear Nose Throat J. 2007;86:236-237.
- Raza SN, Rahat ZM. Horner's syndrome as a co-presentation of tuberculous retropharyngeal abscess. J Coll Physicians Surg Pak. 2010;20:279-281.
- Philpott CM, Selvadurai D, Banerjee AR. Paediatric retropharyngeal abscess. J Laryngol Otol. 2004;118:919-926.
- Singh I, Chanda R, Gupta KB. Fatal pyothorax: a rare complication of retropharyngeal abscess. Indian J Chest Dis Allied Sci. 2003;45:265-268.
- Oktem F, Guvenc MG, Yilmaz S, Edizer DT, Kara B. Asymptomatic retropharyngeal abscess related to cervical Pott's disease. Am J Otolaryngol. 2006;27:278-280.