6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ffa411210000006907000001000200
6go6ckt5b5idvals|845
6go6ckt5b5|2000F757Tab_Articles|Fulltext
Introduction
Acute pulmonary embolism is a component of venous thromboembolism (VTE), which may prove fatal if not suspected and subsequently treated. Incidence of pulmonary embolism is around 0.5-1 case per 1000 cases [
1]. This has been estimated that 70% of proven post-mortem cases of pulmonary embolism are not even suspected during the course of treatment [
2]. On the contrary, only 25-30% of suspected cases turned out to be cases of pulmonary embolism in post-mortem studies [
3]. Young patients are more likely to be mismanaged, as suspicion in healthier young patient is very low, and inspite of various diagnostic modalities high clinical suspicion remains the key for diagnosis.
Case Report
A 30-year-old young male patient, no known co-morbidity, presented to emergency department with history of cough and breathlessness on exertion for 2 days. Initial examination showed respiratory rate: 28/min, pulse: 120/min, blood pressure: 130/80 mm of Hg, SpO2: 88% on room air, temperature: 98.4º F, and scattered wheeze on chest examination. No other significant finding was noted. CT thorax showed peripheral patchy areas of consolidation/atelectasis like changes in right middle and lower lobes and left lower lobe.
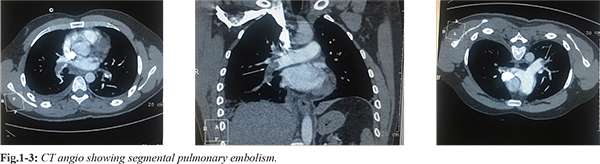
Patient was admitted and shifted to intensive care unit. He was managed with broad spectrum antibiotics, antipyretics, fluids, oxygen and supportive care. His symptoms started to worsen; he had tachypnea, persistent hypoxemia. 2D echocardiography showed mild mitral and tricuspid regurgitation with ejection fraction 55%, right ventricular systolic pressure (RVSP) 55 mmHg. His bilateral lower limb venous Doppler was done which did not show any evidence of deep venous thrombosis. CT pulmonary angiography was done which showed moderate pulmonary thromboembolism with evidence of hypodense thrombus seen at ramification of bilateral pulmo-nary arteries (right>left) extending in to segmental branches [Fig.1-3]. Patient was started on low molecular weight heparin. Despite four days of low molecular weight heparin therapy patient was still having high oxygen requirement and persistent tachypnea along with hemoptysis and hematuria. His repeat 2D echocardiography showed RVSP 65 mm of Hg. Now intra-arterial thrombolysis was done with reteplase. Patient symptoms started to improve, repeat 2D echocardiography showed RVSP of 45 mm Hg. Subsequently, patient was discharged on oral anti-coagulants.
Discussion
Pulmonary embolism is common and potentially lethal condition. Most patients who succumb to pulmonary embolism do so within the first few hours of the event. Despite diagnostic advances, delays in pulmonary embolism diagnosis are common and represent an important issue [
6]. As a cause of sudden death, massive pulmonary embolism is second only to sudden cardiac death.
The risk of blood clots is increased by cancer, prolonged bed rest, smoking, stroke, certain genetic conditions, estrogen-based medication, pregnancy, obesity, and after some types of surgery [
4]. About 90% of emboli are from proximal leg DVTs or pelvic vein thromboses. Clinically apparent DVT is present in only 11% of confirmed cases of pulmonary embolism. The classic presentation of PE is the abrupt onset of chest pain, breathing difficulty and hypoxia but some patients may have no obvious symptoms at presentation. The diagnosis of pulmonary embolism should be suspected in patients with respiratory symptoms unexplained by an alternative diagnosis. Evidence-based literature supports the practice of determining the clinical pre-test probability of pulmonary embolism before proceeding with diagnostic testing [
4]. The three validated systems include the Modified Wells Scoring System, the Revised Geneva Scoring System, and the Pulmonary Embolism Rule out Criteria (PERC) [
5-
7]. Low probability PE can be ruled out with D-dimer testing [
11]. CTPA is the gold standard for diagnosing pulmonary embolism [
12]. When a pulmonary embolism is identified, it is characterized as acute or chronic. In terms of pathologic diagnosis, acute embolus is situated centrally within the vascular lumen and occludes a vessel (vessel cutoff sign) [
12]. Chronic embolus is eccentric and contiguous with the vessel wall, reduces the arterial diameter by more than 50%, evidence of recanalization within the thrombus is present, and an arterial web is present.
The variability of presentation sets the patient and clinician up for potentially missing the diagnosis. Classic presentation of abrupt onset of pleuritic chest pain, shortness of breath, and hypoxia is rarely seen. Studies of patients who died unexpectedly of pulmonary embolism revealed that patients had complained of nagging symptoms, often for weeks, before dying. Forty percent of these patients had been seen by a physician in the weeks prior to their death
Acute pulmonary embolism in young adults is not very uncommon. A young adult presenting with acute onset of dyspnea, pulmonary embolism should be kept a possibility, as most of the time PE is not considered in differential diagnosis while evaluating such patients in emergency. Most of young patients reported in literature are young females, either pregnant or on oral contraceptives. Pulmonary embolism requires high clinical suspicion, based on validated scores and requires further multi-modality investigation to confirm or rule out disease.
Conclusion
Unlike infectious diseases, cardiac disorder or blood disorder, no specific symptoms, signs or investigations reflect pulmonary embolism immediately. Hence young male presenting with acute onset of dyspnea should be evaluated for common cause of dyspnea but pulmonary embolism should be kept in mind, so as not to miss this fatal disease.
Contributors: CC: manuscript writing, patient management; GMM: manuscript editing, patient management; DN: critical inputs into the manuscript. GMM will act as guarantor. All authors approved the final version of this manuscript.
Funding: None; Competing interests: None stated.
References
- Heit JA. The epidemiology of venous thromboembolism in the community. Arteroscler Thromb Vasc Biol. 2008;28:370-372.
- Goldhaber SZ, Hennekens CH, Evans DA, Newton EC, Goldleski JJ. Factors associated with correct antemortem diagnosis of major pulmonary embolism. Am J Med. 1982;73:822-826.
- Rubeinstein I, Murray D, Hoffstein V. Fatal pulmonary emboli in hospitalised patients: An autopsy study. Arch Intern Med. 1988;148:1425-1426.
- Anderson FA Jr, Spencer FA. Risk factors for venous thromboembolism. Circulation 2003;107:9-16.
- Wells PS, Ginsberg JS, Anderson DR, Kearon C, Gent M, Turpie AG, et al. Use of clinical model for safe management of patients with suspected pulmonary embolism. Ann Intern Med. 1998;129:997-1005.
- Elliot CG, Goldhaber SZ, Visani L, De Rosa M. Chest radiography in acute pulmonary embolism. Results from the International Cooperative Pulmonary Embolism Registry. Chest. 2000;118:33-38.
- Ferrari E, Imbert A, Chevalier T, Mihoubi A, Morand P, Baudouy M. The ECG in pulmonary embolism. Predictive value of negative T waves in precordial leads - 80 case reports. Chest. 1997;111:537-543.
- Wells PS, Anderson DR, Rodger M, Steill I, Dreyer JF, Barnes D, et al. Excluding pulmonary embolism at the bedside without diagnostic imaging: Management of patients with suspected pulmonary embolism presenting to the emergency department by using a simple clinical model and d-dimer. Ann Intern Med. 2001;135:98-107.
- Stein PD, Fowler SD, Goodman LR, Gottschalk A, Hales A, Hull RD, et al. Multi detector computed tomography for acute pulmonary embolism. N Engl J Med. 2006;354:2317-2327.
- Kurzyna M, Torbicki A, Pruszczyk P, Burakowska B, Fijalkowska A, Kober J, et al. Disturbed right ventricular ejection pattern as new Doppler echocardiographic sign of acute pulmonary embolism. Am J Cardiol. 2002;90:507-511.
- Cossete B, Pelletier ME, Carrier N, Turgeon M, Leclair C, Charron P, et al. Evaluation of bleeding risk in patients exposed to therapeutic unfractioned or low molecular weight heparin: A cohort study in context of a quality improvement initiative. Ann Pharmacother. 2010;44:994-1002.
- Dalla-Volta S, Palla A, Santolicandro A, Giutini C, Pengo V, Visioli O, et al. PAIMS 2: Alteplase combined with heparin verses heparin in treatment of acute pulmonary embolism. Plasminogen activator Italian multicentre study 2. J Am Coll Cardiol. 1992;20:520-526.