6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ff242c27000000cc07000001000200
6go6ckt5b5idvals|915
6go6ckt5b5|2000F757Tab_Articles|Fulltext
Introduction
Congenital melanocytic nevi (CMN) are loci of concentrated pigment that are visible on the skin and are present at birth. They are benign and result from a defective development of precursor melanocytes in the fetus, consisting of an abnormal mixture of skin elements. Their incidence does not depend on skin color or other racial factors [
1]. They are classified according to the maximum predicted diameter in adulthood (predicted adult size, PAS). CMN with a PAS > 50 cm are classified as giant, and usually appear between the 5th and 24th gestational week with an occurrence of 1:50000 births [
1].
The diagnosis is based on the typical clinical appearance, as they usually appear with a brownish hue and may have abnormal or geographical borders, flat or protruding surface and hypertrichosis (hair). The infected areas are characterized as “cape”, “bathing trunk”, “tippet” or “garment”, according to their distribution. Their depth can be a few mm under the epidermis or they can expand as far as the subcutaneous tissues; they may have any size, covering any part of the body. In 75% of the cases CMNs are accompanied by small, multiple lesions called “satellites”. These lesions can be present at birth and/or may proliferate significantly during the first years of life. Their number must be recorded, because a number > 20 is connected to neurological abnormalities [
1-
4].
Inspite of their great rarity, their diagnosis is important, as they have predisposition for development of dermal or extra-dermal melanoma [
1,
2,
3]. Every patient with a giant CNM should be considered a suspect for development of neurodermal melanosis regardless of the fact that he may or may not present neurological symptoms and MRI brain and the spinal marrow is advisable before the myelination of the brain [
1,
4,
5]. The management of each case must be individualized. The treatment consists of surgical operations, non-surgical procedures and psychological support of patients and family, as well as lifelong monitoring.
Case Report
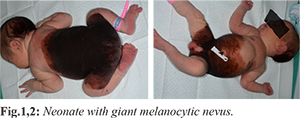
A male neonate was born from 34 year old para 1 mother, via a cesarean section (according to mother’s wish) at 38 weeks gestational age. Both parents were healthy and there was no significant family history. The neonate’s weight at birth was 3900 grams, the head circumference was 37.7 cm and the body length was 54 cm. The neonate had a giant melanocytic nevus of a brownish hue with geographical borders, flat surface and multiple satellite lesions. Specifically it had a giant melanocytic nevus of a “bathing trunk” distribution with 20 cm diameter on the anterior surface of the trunk and 24 cm on the posterior surface, extending to the anus, as well as multiple satellite lesions (>20) on the limbs (6 cm maximum diameter). The main lesion was of a developed constitution with a pronounced thickening and wrinkling; it lacked uniformity in color and did not have definite borders. Multiple papules with definite borders and dark, black color were present on the posterior surface of the trunk [Fig.1,2]. The objective examination of the other systems was normal. The neonate was assessed by a dermatologist and a plastic surgeon, whereas the pediatric neurologic assessment did not present any pathology. Ultrasound abdomen, ultrasound and MRI of the brain did not show involvement of systemic system. The pediatric neurologic assessment at ten months was normal and new satellites had emerged.
Discussion
The giant CMN are evident at birth, more usually covering one side of the body, and more rarely the head, the neck and the limbs. Relevant to the CMN disorders are neurocutaneous melanosis and melanoma [
1,
2,
3]. Neurocutaneous melanosis (NCM) is a neurological and cutaneous disorder characterized by a non-normal concentration of melanocytes inside the CNS and the skin. Giant CMN was first described by Rokitanski in 1861 in adolescent female with hydrocephalus and developmental retardation; and after her death meningeal melanocytosis was found [
1,
6]. Neurocutaneous melanosis is a complication of large and giant CMN or of multiple small ones. Kadorega and Friedento defined coexistence of a large melanocytic nevus or of multiple ones (>3) with meningeal melanocytosis or melanoma, without signs of cutaneous melanoma [
1]. MRO scan of the brain and the spinal marrow is advised in giant CMN and >20 satellite nevi, as these individuals have greater probability to have NCM [
1,
4,
5,
7,
8]. Individuals with giant CMN and PAS >40 with large and giant CMN on the back, on the neck or on the head are in increased danger for NCM even in absence of melanoma, inspite of the fact that many symptomatic patients survive with various neurological defects [
6].
About half of the individuals with NCM will become symptomatic before the age of 5 years. Possible symptoms are hydrocephalus or other signs indicating increased intracranial pressure, like headaches, vomiting or seizures [
6]. Mild to severe developmental retardation and non-normal muscular tone have been described. In bibliography there is a report of a primary intracranial melanoma in child with a giant CMN and a normal MRI [
4]. The cutaneous melanoma tends to penetrate deep in the skin or in the fat tissue of the LCMN, rendering the early diagnosis difficult. MRI brain is advisable in multiple CMN or one CMN with more than 20 satellite nevi [
1,
4,
7]. Also, every patient with newly appearing neurological symptoms, like urination, tip-toe walking, epilepsy and sunset sign must undergo neurological evaluation and suitable imaging. Symptomatic neurocutaneous melanosis even without malignancy has an extremely poor prognosis.
It is important to diagnose the intracranial lesions at birth as this contributes to an earlier diagnosis of clinical manifestations. Knowledge of these lesions facilitates the differential diagnosis of melanotic loci that are part of the disease or secondary metastases of a malignant exchange of a giant CNM. It is not always feasible to make a differential diagnosis of primary melanoma or metastatic lesions via MRI [
6]. It has to be noted that non-participation of the meninges does not exclude the neurocutaneous melanosis or melanoma [
4]. Inspite of the fact that the neurocutaneous melanosis is better imaged via MRI, the brain ultrasound is quite useful in early diagnosis in neonates [
6]. However, ultrasound does not visualize very small lesions in the cerebellum, due to the artifacts of the bones [
6].
The therapeutic approach of patients with giant CMN consists in plastic surgery techniques aiming at the replacement of the skin in all its thickness, whereas the sole monitoring is the choice for non-accessible and homogeneous melanocytic nevi [
1,
2]. Treatment must be individualized. Psychological support is advised for all patients and their families, regardless of the therapeutic choice. Therapies that are under investigation are being developed. Lifelong monitoring is necessary for patients with large and giant melanocytic nevi, regardless of the treatment adopted.
Conclusion
Congenital melanocytic nevi have a characteristic clinical appearance at birth. Although rare, their early diagnosis is necessary due to sinister nature of disease. Treatment should be individualized. Lifelong monitoring of these patients is necessary.
Contributors: FB: manuscript writing, patient management; TP, AD: manuscript editing, patient management; VG: critical inputs into the manuscript. VG will act as guarantor. All authors approved the final version of this manuscript.
Funding: None; Competing interests: None stated.
References
- Price H, Etchevers H. Giant congenital melanocytic nevus. Available at: rarediseases.org /rare-diseases/giant-congenital-melanocytic-nevus/. Accessed on 23rd December 2018.
- Viana AC, Gontijo B, Bittencourt FV. Giant congenital melanocytic nevus. An Bras Dermatol. 2013;88:863-878.
- Viana AC, Goulart EM, Gontijo B., Bittencourt FV. A prospective study of patients with large congenital melanocytic nevi and the risk of melanoma. An Bras Dermatol. 2017;92:200-205.
- Al-Hadithy N, Al Nakib K, McGurk S, Quaba A. Primary intracranial melanoma in a child with a giant congenital naevus and normal MRI. BMJ Case Rep. 2013;2013:bcr2013009276.
- Scattolin MA, Lin J, Peruchi MM, Rocha AJ, Masruha MR, Vilanova LC. Neurocutaneous melanosis: follow-up and literature reviw. J Neuroradiol. 2011;38:313-318.
- Yakut ZI, Bas AY, Turan A., Demirel N., Demirkan TH. Early sonographic diagnosis of neurocutaneous melanosis in a newborn. Iran J Radiol. 2014;11:e10107.
- Kinsler VA, Aylett SE, Coley SC, Chong WK, Atherton DJ. Central nervus system imaging and congenital melanocytic naevi. Arch Dis Child. 2001;84:152-155.
- Leech SN, Bell H, Leonard N, Jones SL, Geurin D, McKee PH, et al. Neonatal giant congenital nevi with proliferative nodules. Arch Dermatol. 2004;140:83-88.