6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ff684b27000000e006000001000400
6go6ckt5b5idvals|917
6go6ckt5b5|2000F757Tab_Articles|Fulltext
Introduction
Tuberculosis remains one of the major health problems in the developing countries due to malnutrition, poor socioeconomic status and immunodeficiency syndromes. Skeletal tuberculosis represents a rare form of tuberculosis, accounting for only 1-2 per cent of the cases. Primary calvarial tuberculosis with no evidence of tuberculosis elsewhere is still rarer and accounts for only 0.2 to 1.3% of cases of skeletal tuberculosis.
Osteolytic lesions of skull bones may closely mimic the skull bone metastasis, multiple myeloma and conventional radiographs are often inconclusive. Moreover, tuberculoma of the skull might be difficult to diagnose when the patient has no evidence or history of tuberculous infection. A high index of suspicion is important to recognize tuberculous involvement of the skull. Biopsy in these cases confirms the diagnosis.
Case Report
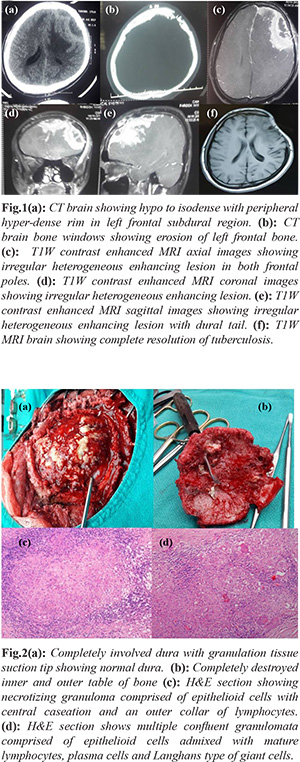
A 20 year old male presented with history of gradually progressive headache, associated with multiple episodes of vomiting and generalized tonic-clonic seizures. She did not have any history of fever or any other constitutional symptoms. On examination, there was no localized scalp swelling or draining sinuses. Complete blood picture, chest X-ray, liver function tests, renal function tests, all were within normal limits. Computed tomography scan of the brain revealed hypo to iso-dense lesion in left frontal convexity with irregular erosions of inner table of frontal bone with bone perforation. Magnetic resonance imaging (MRI) brain revealed a 9×3 cm sized heterogeneously enhancing extra-axial bi-frontal convexity mass lesion, more on the left side than right side with midline shift of 7 mm. Intra-operatively, subcutaneous tissue was found to be densely adherent to the frontal bone. The dura was thickened and adherent to the bone that was punched out at various places. Some part of frontal lobe parenchyma was also infiltrated by the lesion. The lesion was excised en-bloc along with involved dura and bone. Post-operative period was uneventful. Histopathology showed extensive areas of necrosis and many caseating as well as non-caseating well defined epithelioid granulomas with admixed foreign body and Langhans type of giant cells. Lymphocytic cuff surrounded the granulomas. Tissue was submitted for culture but didn’t yield any growth. Based on the histopathology, a final diagnosis of tubercular osteomyelitis of skull was made and patient was started on anti-tuberculous treatment. Follow up imaging after one year revealed complete resolution of tuberculoma.
Discussion
Calvarial tuberculosis was first described by Reid et al. in 1842 [1]. Children are commonly affected, 75-90% cases are less than 20 years of age [1]. Patients usually present with painless swelling of the scalp and discharging sinuses; seizures and motor deficits are rare presentations [1-3]. Our patient presented with generalized tonic-clonic seizures associated with headache and vomiting. In contrast to the usual presentation of these patients, there was no scalp swelling or draining sinuses in our case.
Tuberculous skull osteomyelitis usually occurs through the hematogenous spread of bacilli from primary active focus in the lungs or latent infection [2]. However, in our case, on clinical examination and investigations, no active focus of tuberculosis was found. Many authors have hypothesized that trauma and increased vascularity are contributing factors [1,2]. Meng et al, however, had challenged the significance of trauma, as they found no patients with a history of head injury. In our case either, patient did not reveal any such history of trauma, thus supporting findings by Meng et al. Involvement of inner table associated with formation of extra-dural granulation tissue may present as headache localized at the site of infection and focal neurological deficits which explains our patient’s presentation with headache and seizures [1,2].
Diagnosis of calvarial tuberculosis is challenging and is often not suspected because of its rarity. On imaging, there are no specific diagnostic criteria to diagnose the tuberculous osteomyelitis. Plain X-ray skull can show rarification in early cases which later on turns into punched out defect. CT brain shows bony destruction and degree of parenchymal and meningeal involvement and presence of extra-dural soft tissue [1]. MRI is more sensitive in detecting changes in meninges and brain parenchyma [2]. As tuberculous lesions are osteolytic and can be multiple, they need to be differentiated from the multiple myeloma, metastasis, and Ewing’s sarcoma. High index of suspicion and knowledge is required for diagnosis of tuberculous osteomyelitis. Anti-tubercular (ATT) treatment is choice of treatment for small lesions after confirming diagnosis by non-invasive methods. Surgery is indicated to establish diagnosis, remove extra-dural granulation tissue and destroyed bone, to relieve mass effect.
Conclusion
Although calvarial tuberculosis is rare even in endemic areas with tuberculosis but it has good prognosis after treatment. Treatment modality is predominantly ATT medication, which may be given as per the Revised National Tuberculosis Control Programme. Surgical intervention may be considered for large epidural symptomatic patients.
Contributors: VRK: manuscript writing, patient management; RK: manuscript writing, histopathology; RT, SSM, CS: manuscript editing, histopathology; SK: critical inputs into the manuscript, discussion, imaging. VRK will act as guarantor. All authors approved the final version of this manuscript.
Funding: None; Competing interests: None stated.
References
- Meng CM, Wu YK. Tuberculosis of the flat bones of vault of skull. J Bone Joint Surg Br. 1942;24:341-353.
- Mohanty S, Rao CJ, Mukherjee KC. Tuberculosis of the skull. Int Surg. 1981;66:81-83.
- Reddy RD, Ram Mohan S, Chari SK, Satyanarayana K. Tubercular osteomyelitis of the skull. Indian J Tuberc. 1974;21:213-215.
- Tirona JP. The roentgenological and pathological aspects of tuberculosis of the skull. Am J Roentgenol Radium Ther Nucl Med. 1954;72:762-768.
- Miles J, Hughes B. Tuberculosis osteitis of the skull. Br J Surg. 1970;57:673-679.
- Sharma R, Tyagi I, Kumar R. Phadke RV. Tuberculosis of the skull. A case report and review of the literature. Neurosurgery Rev. 2000;23:103-106.
- Nemir RL, Branom Geneses N, Balasubramanyam P. Extensive sclerosis of the bone of the skull due to primary nasal tuberculosis. Pediatric Radiol. 1976;8:42-44.
- Bhandari B, Mandowara SL, Joshi H. Tubercular osteomyelitis of the skull. Indian J Paediatr. 1981;48:113-115.
- Jadhav RN, Palande DA. Calvarial tuberculosis.Neurosurgery. 1999;45:1345-1348.
- Raut AA, Nagar AM, Muzumdar D, Chawla AJ, Narlawar RS, Fattepurkar S, et al. Imaging features of calvarial tuberculosis: A study of 42 Cases. AJNR Am J Neuroradiol. 2004;25:409-414.
- Patankar T, Varma R, Krishnan A, Prasad S, Desai K, Castillo M. Radiographic findings in tuberculosis of the calvarium. Neuroradiology. 2000;42:518-521.
- Diyora B, Kumar R, Modgi R, Sharma A. Calvarial tuberculosis: A report of eleven patients. Neurol India. 2009;57:607-612.