6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ff24a9270000006407000001000a00
6go6ckt5b5idvals|923
6go6ckt5b5|2000F757Tab_Articles|Fulltext
Introduction
Separation of intima and medial layers of aorta due to tear in the intima layer is known as acute aortic dissection (AAD). Incidence of AAD is only 2.6 to 3.5 per 100,000 general population and is mostly diagnosed post mortem [
1]. Young adults with Marfan syndrome usually die as a result of aortic dissection [
2]. The mortality rate of AAD increases by 1% to 2% per hour if not detected and treated on time [
3].
Diagnosing AAD is challenging in the emergency department due to its diversified presentations. Studies reveal that around 38% of AAD are missed on initial evaluation [
4]. It is not only a life threatening condition in itself but also mimics other life threatening conditions like acute coronary syndrome (ACS), pulmonary embolism or strokes at presentation, which can lead to delay in diagnosis and mortality [
5]. Classically patients with aortic dissection present with retro-sternal chest pain which is ripping/tearing in character [
6]. We present an unusual case of a 28 year old male with Marfanoid habitus presenting to our emergency department (ED) with dizziness and was diagnosed as acute aortic dissection.
Case Report
A 28 year old known scoliotic male was brought to our ED with complaints of dizziness followed by one episode of vomiting. On presentation patient was conscious and coherent having no neurological deficits with blood pressure of 100/60 mmHg, pulse rate of 72/minute, respiratory rate of 20/minute, temperature of 98.7º F, oxygen saturation of 99% on room air and blood glucose of 135 mg/dL. Systemic examination was significant for a diastolic murmur and an absent right radial pulse. The patient had long thin arms, legs and fingers and had a pigeon chest. Rest of the systemic examination was unremarkable. Past surgical history was significant for repeated fractures to left forearm due to trivial traumas in his childhood. Patient was suspected to be having Marfan syndrome.
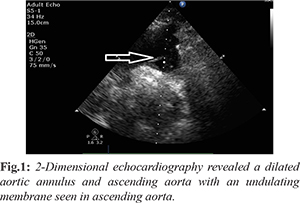
His initial blood work showed an increased total leucocyte count (TLC) count of 15,700/µL. Rest of the blood was unremarkable. An initial electrocardiograph (ECG) showed slight upsloping of ST segment in inferior leads and hence a 2-dimensional echocardiography (2D echo) was ordered to rule out ACS. The 2D echo revealed a dilated aortic annulus and ascending aorta with an undulating membrane seen in ascending aorta arising from left coronary sinus with non-coapting leaflets with severe aortic regurgitation suggestive of acute aortic dissection [Fig.1].
On retaking the history, the patient never complained of any chest pain or back pain at any moment. The patient immediately underwent a Computed Tomography Angiography (CTA) of the aorta which demonstrated aneurysmal dilatation of aortic root and associated dissection of the aortic root, with type A dissection of aorta extending into origin of the arch vessels and brachiocephalic trunk, common carotid artery and left subclavian artery and abdominal aorta [Fig.2-3]. The patient soon after CTA became hemodynamically unstable with a blood pressure of 80/60 mm Hg, respiratory rate of 35/min and became drowsy. He was immediately intubated and ventilated, started on fluids and noradrenaline infusions. Urgent cardiothoracic consult was sought and the patient was immediately shifted to the operating room with a diagnosis of acute type A aortic dissection. The patient underwent urgent Bentall procedure and discharged in a stable condition after 17 days.
Discussion
We have discussed a case of painless aortic dissection with an uncommon complaint of dizziness in a young patient with possible Marfan syndrome (MFS). Aortic dissection was first described by Morgagni almost 200 years ago [
7]. Aortic dissection can propagate to involve the distal part of the aorta, or extend to involve different branches, such as the carotid, subclavian and renal arteries or spread in a retrograde fashion to involve the coronary arteries [
8].
According to the Stanford classification, type A dissections involve the ascending thoracic aorta, whereas type B dissections involve the descending aorta [
9]. The etiology for ascending aortic root aneurysm in young populations may be associated with connective tissue disorders such as MFS, Ehlers-Danlos syndrome and bicuspid aortic valve disease. Other factors include infection, inflammation, trauma and idiopathic [
10]. MFS being an autosomal dominant disorder is one of the most common inherited disorders of the connective tissue. It has a prevalence of 1 in 5000 individuals with variable phenotypic expression. Most patients of MFS harbor mutations involving the FBN1 gene encoding the connective tissue protein fibrillin-1 [
11]. MFS is present in 4.95% of cases of aortic dissections.
A transthoracic 2D echocardiography is a valuable bedside test performed non-invasively, to look for aortic root dilatation, presence of aortic valvular regurgitation and the function and dimensions of left ventricle [
12]. CT angiography is the first imaging modality with very high sensitivity (100%) and specificity (98%) that evaluates entire aorta and aortic branches effectively and hence has become the gold standard. The main disadvantage of CTA is the need for contrast administration and radiation exposure which is not the optimal test for hemodynamically unstable patients [
13]. Early surgical intervention is the mainstay of treatment for all type A dissections [
14].
Ascending aortic dissection is a rare but fatal condition where one needs to be proactive in identifying the condition. Missing the diagnosis might prove fatal within minutes to hours of presentation. Identifying AAD with atypical presentation is a challenging task particularly for emergency physicians. Patients with suspected Marfan syndrome or other connective tissue disorders should warrant a low threshold to investigate towards establishing a diagnosis of AAD and prevent fatalities.
Contributors: AKK: participated in the patient care, and writing the paper. AV, WRS: patient care, manuscript writing. MH, AS and SJ participated in revising the manuscript critically and contributed towards writing discussion. AKK will act as guarantor. All authors approved the final version of this manuscript.
Funding: None; Competing interests: None stated.
References
- Clouse WD, Hallett JW Jr, Schaff HV, Spittell PC, Rowland CM, Ilstrup DM, Melton LJ. Acute aortic dissection: population-based incidence compared with degenerative aortic aneurysm rupture. 3rd Mayo Clin Proc. 2004;79:176-180.
- Mészáros I, Mórocz J, Szlávi J, Schmidt J, Tornóci L, Nagy L, et al. Epidemiology and clinic pathology of aortic dissection. Chest. 2000;117:1271-1278.
- Zalzstein E, Hamilton R, Zucker N, Diamant S, Webb G. Aortic dissection in children and young adults: diagnosis, patients at risk, and outcomes. Cardiol Young. 2003;13:341-344
- Coady MA, Rizzo JA, Goldstein LJ, Elefteriades JA. Natural history, pathogenesis, and etiology of thoracic aortic aneurysms and dissections. Cardiol Clin. 1999;17:615-635.
- Spittell PC, Spittell JA Jr, Joyce JW, Tajik AJ, Edwards WD, Schaff HV, et al. Clinical features and differential diagnosis of aortic dissection: experience with 236 cases (1980 through 1990). Mayo Clin Proc. 1993;68(7):642-651.
- Sheikh AS, Ali K, Mazhar S. Acute aortic syndrome. Circulation. 2013;128:1122-1127.
- Verma A, Sheikh WR, Jaiswal S. An atypical presentation of acute aortic dissection in the Emergency Department. J Case Reports. 2017;7:177-179.
- Nienaber CA, Fattori R, Lund G, Dieckmann C, Wolf W, von Kodolitsch Y, et al. Nonsurgical reconstruction of thoracic aortic dissection by stent-graft placement. N Engl J Med. 1999;340:1539-1545.
- Hagan PG, Nienaber CA, Isselbacher EM, Bruckman D, Karavite DJ, Russman PL, et al. The International registry of acute aortic dissection (IRAD). New insights into an old disease. JAMA. 2000;283:897-903.
- R Cohen, D Mena, R Carbajal-Mendoza, O Arole, JO Mejia. A case report on asymptomatic ascending aortic dissection. Int J Angiol. 2008;17:155-161.
- Naidoo P, Ranjith N, Zikalala Z, Mahoney S, Ho K. Marfan syndrome: a case report and pictorial essay. Pan Afr Med J. 2018;30:171.
- Evangelista A, Flachskampf FA, Erbel R, Antonini-Canterin F, Vlachopoulos C, Rocchi G, et al. Echocardiography in aortic diseases: EAE recommendations for clinical practice. European Journal of Echocardiography. 2010;11:645-658.
- McMohan MA, Squirrell CA. Multidetector CT of aortic dissection: A pictorial review. Radiographics. 2010;30:445-460.
- De Sanctis RW, Doroghazi RM, Austen WG, Buckley MJ. Aortic dissection. N Engl J Med. 1987;317:1060-1067.