6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ff5473050000008f02000001001200
6go6ckt5b5idvals|295
6go6ckt5b5|2000F757Tab_Articles|Fulltext
Introduction
Multiple primary tumors (MPMs) are defined as two or more malignancies in a single individual without any relationship between cancers [
1]. It is not very rare, with observed increase in their incidence which can be explained by the greater awareness, improved diagnostic techniques and facilities [
2], firstly described by Billroth at the end of the 19th century [
3]. One of the earliest statistical analyses of MPMs was carried out by Bugher in 1934 [
4]. In this report we present two cases with double primary tumors; first one is colonic cancer and metachronous thyroid cancer; second case with colon cancer and metachronous breast cancer.
Case Reports
Case 1:
82 years old female patient was referred to our center (King Abdullah Medical Center; Holly Capital) as a case of acute abdomen. The illness started 2 months prior to admission with constipation of gradual onset having progressive course associated with nausea and vomiting till complete obstruction.
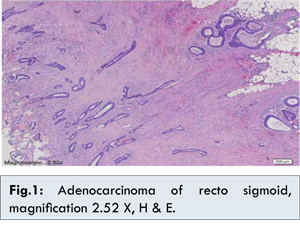
There were past history of diabetes mellitus type II with patient on oral hypoglycemic medications since last 2 years and open cholecystectomy was performed ten years ago due to gall stones. Family history was irrelevant. On physical examination, her abdomen was distended and tender on palpation. There was palpable mass in left iliac region, and bowel sounds were not audible. On laboratory testing, she had a serum chemistry panel and complete blood count within normal limits. Computed tomography scan revealed colo-rectal mass causing complete intestinal obstruction. Urgent laparotomy was done with resection of colonic mass and diverting colostomy. Histological examination revealed moderately differentiated adenocarcinoma of 3 cm tumor size invading through the muscularis propria into the pericolic fat, both peri-neural or lympho-vascular invasion were not identified and there was one lymph node positive out of seven [Fig.1].
The patient had a smooth recovery and was discharged home 10 days after operation. Post-operative evaluation and staging by computed tomography scan to chest, abdomen and pelvis revealed no evidence of residual or distance spread of tumor. She was started on capcitabine as adjuvant treatment and completed 8 cycles without serious complications. 3 months later, computed tomography scan to chest, abdomen and pelvis as a part of follow up revealed left thyroid nodule measured 2.6x1.2 cm with multiple cystic areas inside [Fig.2].
Fine needle aspiration cytology from it revealed papillary carcinoma; at that time she was transferred to head and neck combined clinic for further management. Total thyroidectomy was done and histological examination revealed left thyroid lobe papillary carcinoma, follicular variant with negative surgical margins and lymphovascular invasion. Right thyroid lobe and isthmus revealed multinodular goiter [Fig.3].
Whole body iodine scan showed residual functioning thyroid tissue in the right lobe bed and regional lymph nodes without evidence of distant metastasis. Then she received ablative dose of radioactive iodine 131 with 30 mCi. Now she is under follow up in outpatient clinic with L- thyroxin therapy and calcium supplementation with acceptable general condition.
Case 2:
A 61-years-old female patient was transferred to our oncology center as a case of colon cancer for further management. Her condition started 2 months back by intermittent diarrhea alternating with rectal bleeding associated with abdominal pain, progressing from the upper to the lower abdomen, and weight loss. The condition was neglected and progressed till the patient attended her nearest hospital where she presented with repeated vomiting and abdominal distension. Clinical examination revealed a distended, tender abdomen and inaudible bowel sounds.
Computer tomography (CT) with intravenous contrast showed malignant stricture sigmoid colon with proximal colonic dilatation. At routine laboratory tests, no alterations of the principal biochemical parameters were found. Urgent laparotomy with right hemi-colectomy and end to end anastomosis was performed with uneventful post-operative period. Histopathology examination revealed colon cancer. There was past history of diabetes mellitus for 5 years, with patient on oral hypoglycaemic medications with irrelevant family history.
In our centre, we upload the CT abdomen which revealed malignant stricture sigmoid colon with proximal colonic dilatation [Fig.4]. Histopathology showed; moderately differentiated adenocarcinoma infiltrating the entire thickness of the wall and adjacent pericolic fat, perivascular and perineural invasion were present and three out of six lymph nodes were positive for metastasis 3/6 [Fig.5].
Post-operative reassessment was free from local recurrence or metastatic spread beside normal routine laboratory tests (CBC, biochemical parameters and CEA). So we diagnosed the case as colon cancer stage III for adjuvant chemotherapy. She received 6 cycles of FOLFOX. From that time; she was under regular follow up in oncology centre for next 8 months when small right breast mass about 2x2 cm was discovered accidently. Bilateral mammogram and complementary breast ultrasonography (US) revealed small right breast mass 1.5x1.5 cm with microclacification; highly suspicious of malignancy [Fig.6].
Right breast lumbectomy with right axillary sentinel lymph nodes were done and showed Invasive duct carcinoma grade II. Surgical margins, lymphovascular and perineural invasion; all were negative. Estrogen and progesterone receptors were moderately positive with HER-2 negative [Fig.7].
So we diagnosed the case as breast cancer stage I with intermediate risk, she received 4 cycles of adjuvant chemotherapy (AC×4) last dose at June 2013, followed by adjuvant radiotherapy and now on adjuvant hormonal therapy. Now she is under regular follow up in outpatient clinic in our oncology centre with good general condition.
Discussion
Multiple primary tumors (MPMs) may be synchronous or metachronous depending on the interval between their diagnosis. Synchronous cancers are second tumors occurring simultaneously or within 6 months after the first malignancy, while metachronous multiple malignancies are secondary cancers that developed after more than 6 months after from the first malignancy [
5]. Three diagnostic criteria have been proposed for MPMs: 1) each tumor must present definite features of malignancy, 2) each must be distinct, and 3) the chance of one being a metastasis of the other must be excluded [
6].
MPMs are classified into four types: 1) multicentric, if the two distinct carcinoma arise in the same organ or tissue; 2) systemic, if they arise on anatomically or functionally allied organs of the same system, 3) paired organs, as in the breasts, and 4) random, if they occur as a co-incidental or accidental association in unrelated sites [
7]. Its frequency varies from 0.7% to 14.5% [
8-
12].
Causal mechanisms of multiple primary cancers include genes, the environment, treatment effects, and combinations of these three mechanisms. When researchers focus on genes as causal mechanisms, they often concentrate on cases diagnosed earlier in life [
12]. Although bladder and prostate carcinoma can coexist in the same individual frequent enough [
13,
14], the combination of colon carcinoma with either thyroid carcinoma or breast carcinoma are uncommon. In our cases, there was no clear family history, no predisposing factors or causal factors for each malignancy. It was important to establish the primary nature of both tumors because therapy for these two conditions differs significantly.
The prognosis of patients with MPMs can be determined independently by the stage of each malignancy. The surgical treatment of choice for metachronous multiple primary malignancies are curative resection of each malignant tumor in condition that they are both operable and resectable [
15]. In the reported cases we discovered the metachronous malignancy accidentally during the regular follow up and fortunately they were in early stage which gave us the chance for curative treatment.
A large population base is needed for research on multiple primary cancers; such a population base will require extensive collaboration between cancer registries.
Conclusion
The diagnosis of cancer should not exclude the existence of other concomitant malignancy; especially in patients more than the sixth decade of age as therapy for these two conditions differs significantly.
References
- Yhim HY, Kim HS, Lee NR, Kwak JY, Yim CY. Quadruple primary malignancies of liver, bladder, lung and stomach in one patient. Tumori. 2010;96:787-791.
- Morgenfeld EL, Tognelli F, Gil Deza E, et al. Synchronous and metachronous second (ST) and, third (TT) primary tumors (PT) in a large patient population. Proc ASCO. 2003;22:3152.
- Billroth T. Die allgemeinechirurgischepathologie und therapie in 51 vorlesungen. In: Reimer G, (editor). Handbuchfürstudierende und ärzte.Berlin; 1882.pp. 908.
- Bugher JC. The probability of the chance occurrence of multiple malignant neoplasms. Am J Cancer. 1934;21:2309-2824.
- Suzuki T, Takahashi H, Yao K. Multiple primary malignancies in the head and neck: a clinical review of 121 patients. Acta Otolaryngol Suppl. 2002;547:88-92.
- Warren S, Gates O. Multiple primary malignant tumors: A survey of the literature and a statistical study. Am J Cancer. 1932;16:1358-1414.
- Moertel CG. Multiple primary malignant neoplasms: historical perspectives. Cancer 1977; 40(4 Suppl):1786-1792.
- Alhilli F, Das NS. Cancer in the Arabian Gulf Kingdom of Bahrain (1952-2004). Bahrain Med Bull. 2010;32:57-60.
- Beisland C, Talleraas O, Bakke A. Multiple Primary Malignancies in Patients with Renal Cell Carcinoma; A National Population-Based Cohort Study. BJU Int. 2006;97: 698-702.
- Hayat MJ, Howlander N, Reichman ME. Cancer Statistics, Trends, and Multiple Primary Cancer Analysis from the Surveillance, Epidemiology, and End Results (SEER) Program. Oncologist. 2007;12:20-37.
- Mariotto AB, Rowland JH, Ries LAG. Multiple Cancer Prevalence: A Growing Challenge in Long-Term Survivorship. Cancer Epidemiol Biomarkers Prev. 2007;16: 566-571.
- Jefferson KP, Gillatt DA. Hereditary urological cancer syndromes. Nat Clin Pract Urol. 2007;4:218-226.
- Orhan O, Gerald F, Carmen A, Raymond M. Incidental detection of synchronous primary tumours during staging workup for prostate cancer, Swiss Med Wkly. 2010;140(15-16):233-236.
- Lee SH, Chang PL, Chen SM, Sun GH, Chen SM, Sun GH, et al. Synchronous primary carcinomas of the bladder and prostate Asian J Androl. 2006;8(3):357-359.
- Yoshino K, Asanuma F, Hanatani Y, Kumai K, Ishibiki K. Statistical studies on multiple primary cancers including gastric cancers. Gan No Rinsho. 1984;30(12 Suppl):1514-1523.