Introduction
CCAM (congenital cystic adenomatoid malformation) or congenital pulmonary airway malformations represent rare spectrum of congenital lung abnormality. These result from aberrant lung development at 7th to 17th week of gestation resulting in cystic or solid overgrowth of tubular bronchiolar structure excluding alveoli. The incidence of CCAM (congenital cystic adenomatoid malformations) range between 1:8000 to 1:35,000 live births [
1,
2]. These anomalies are usually detected antenatally or postnatally in infancy and early childhood [
2].
Case Report
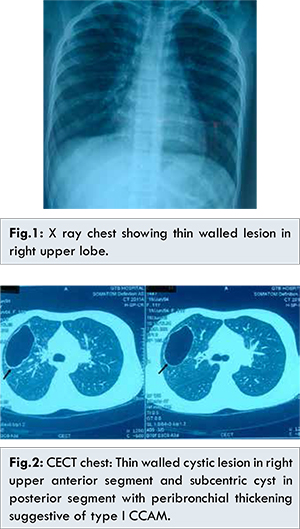
A 11 year female presented with complaints of intermittent fever, dry cough, chest pain for one month and fast breathing for 5 days. On examination there was no pallor, cyanosis, clubbing or lymphadenopathy. Her chest examination revealed resonant note bilaterally with decrease air entry on right side, rhonchi and crepitations predominantly on right side. Her cardiovascular and abdominal examination revealed no abnormality. There was no history of similar illness, tuberculosis or hospitalisation in past. Her hemogram revealed haemoglobin: 14 gm%, total leukocyte count: 6300 mm3, and chest X-ray revealed thin walled lesion in right upper zone [Fig.1]. She received oxygen, 3rd generation cephalosporin and vancomycin. Her blood culture came sterile. She became afebrile on day 4 of hospitalisation but continued to have decreased breath sound on right side, so she was evaluated for other possible cause including tuberculosis, congenital lung malformation, and cavitatory lung lesion. Her Mantoux was not reactive, sputum was AFB negative and sterile. Her CECT chest [Fig.2] revealed 4.8x2.9 cm thin walled cystic lesion in right upper anterior segment and subcentric cyst in posterior segment with peribronchial thickening. Subtle ground glass opacity were seen in right middle, posterior and left pericardiac and lingular regions. Cystic lesion suggesting possibility of CCAM type 1 with evidence of superadded infection was the final impression. She received antibiotics for 14 days and later referred for surgical consideration.
Discussion
Congenital cystic adenomatoid malformation, a rare type of congenital lung malformation is result of overgrowth of lung tissue occurring at different stages of lung development. CCAM occurs due to developmental arrest at terminal bronchiolar level (pseudoglandular stage 7-17 week of gestation) followed by proliferation of bronchiole excluding mature alveoli and transformation into heterogeneous cystic or non-cystic areas which are supplied by pulmonary artery, rarely from systemic artery as in hybrid lesions. Based on embryological stage of insult, histology and dominant cyst size, these malformations have been classified into five types (type 0,1, 2, 3 and 4) [
3]. Adzick et al. classified them as macrocystic type (cyst size 5 mm or more, type 1,2) and microcystic type (cyst size < 5 mm, type 3) on the basis of gross anatomy and ultrasound findings [
4].
Type 1 lesions (cyst size more than 2 cm) are most common CCAM (60%-65%) and often occur unilaterally with equal incidence in male and female. Histologically type 1 cysts are lined by pseudo-stratified columnar epithelium and wall is made of fibro-elastic, muscular tissue or rarely has cartilage. Type 2 CCAM (0.5-2 cm) is associated with extrapulmonary malformation. Type 3 CCAM is usually solid and is microcystic lesion with brochioalveolar morphology. Diagnosis can be made in antenatal period by ultrasound, Doppler or MRI and postnatally by chest X-ray or CT chest [3,4]. CECT of our case revealed type 1 CCAM with maximum width of dominant cyst 4.8 cm.
Complications of CCAM include polyhydramnios, hydrops, fetal death, recurrent pneumonia, haemoptysis, pneumothorax, and malignant transformation [
3,
4]. Commonly CCAMs present in infancy or in childhood. Small cystic malformation can regress in the third trimester [1]. Wong et al. [
5] found that one patient (n=35) showed antenatal regression, 40% (n=35) of neonate were symptomatic at birth and 86% became symptomatic at median age of two year (range 1 month-13 years). Our index case presented at 11 year of age. Rarely, they present first time in adolescence and adulthood as case of persistent pneumonia. Surgery is treatment of choice in these lesions.
Conclusion
CCAM represent a rare spectrum of congenital lung malformation. Rarely they can have later age of presentation. Diagnosis is made by chest X-ray and HRCT chest and definitive management is surgery.
References
- Laberge JM, Flageole H, Pugash D, KhalifeS, Blair G, Filiatrault D, et al. Outcome of the prenatally diagnosed congenital cystic adenomatoid lung malformation: A Canadian experience. Fetal Diagn Ther. 2001;16:178-186.
- Nadeem M, Elnazir B, Greally P. Congenital Pulmonary Malformation in Children. Scientifica. 2012;2012:209896.
- Stocker JT. Congenital pulmonary airway malformation: a new name for and an expanded classification of congenital cystic adenomatoid malformation of the lung. Histopathology. 2002;41:424-430.
- Adzick NS, Flake AW, Crombleholme TM. Management of congenital lung lesions. Semin Pediatr Surg. 2002;12:10-16.
- Wong A, Vieten D, Singh S. Harvey JG, Holland AJA. Long-term outcome of asymptomatic patients with congenital cystic adenomatoid malformation. Pediatr Surg Int. 2009;25:479-485.