Introduction
Hypernatremia is defined as a plasma Na+ concentration more than 150 mmol/L (135-145 mmol/L). Hypernatremia is a common clinical problem, observed in 2% hospital inpatients and 15% of patients admitted to the ICU [
1,
2]. Gestational diabetes insipidus (GDI) though a long known entity, very few cases are reported in literature. Herein we describe a young primigravida with GDI.
Case Report
Herein we present a case of post-partum hypernatremia in a 28 year female with pregnancy induced DI, during her third post-partum week. She was referred to us with history of lower segment Caesarean section (LSCS) for meconium stained liquor. She was brought to emergency room with history of weakness for one week, altered sensorium and fever for two days. According to her brother, one week earlier she was at home and apparently healthy, when they noted a questionable fall in bathroom. She received treatment and recovered to normalcy with residual gait disturbance.
In the last two days, she developed fever (Tmax was 1010F) and altered sensorium in the form of irrelevant talk and inconsistent response to verbal commands. A local doctor noted that she had altered sensorium, low platelet count (86,000/cu.mm) with deranged kidney functions (serum creatinine: 2.6 mg/dL) and was referred here. Family denied history of vomiting, loose stools, headache, cough, abdominal pain and seizures. There was no history of diabetes, hypertension, abnormal prenatal period. Baby was apparently doing well.
On clinical examination, she was conscious, obeyed simple commands but had inconsistent response to verbal commands. Her vitals showed a pulse rate of 152/min, blood pressure of 138/70 mmHg, respiration 40/min and saturation of 95% on room air. Neurologic examination revealed a GCS of 14/15 with no obvious weakness, diminished reflexes, flexor plantars and minimal weakness in lower limbs with a power of 3/6. Neck stiffness was strongly positive. Pupils were 3 mm with bilateral sluggish reaction. Rest of systemic examination was within normal limits. Local examination of the LSCS wound showed normal healthy wound with no obvious signs of infection. Arterial blood gas analysis was essentially normal. Random blood sugar was 256 mg/dL. After a litre of normal saline bolus her heart rate reduced to 138/min. Patient was then admitted to ICU with provisional diagnosis of sepsis with cerebral venous thrombosis (CVT) with dyselectrolytemia.
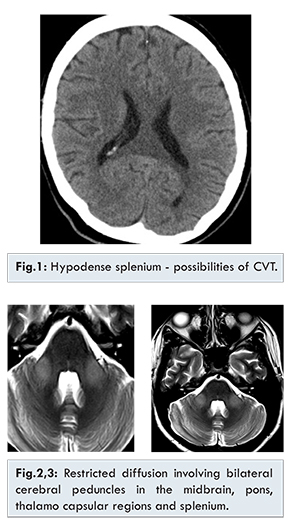
Her initial workup revealed sodium of 179 mmol/L, creatinine of 3.8 meq/L and increased total counts. Investigations for dengue serology, leptospira and malarial parasite were negative. Liver function test and coagulation profile were normal. Urine routine showed increased white blood cell (8-10/cu.mm) and numerous red blood cells. Ultrasound abdomen showed bulky uterus. CT scan of brain showed hypodensity of splenium suggestive of CVT [Fig.1]. Patient was found to have a fluid deficit of 27 liters. She was started on piperacillin/ tazobactum, pantodac, multivitamins and unfractionated heparin (DVT prophylaxis) with sodium monitoring and controlled hydration. MRI revealed hyper-intensities involving bilateral cerebral peduncles in the midbrain, pons, thalamocapsular regions and splenium on diffusion weighted images [Fig.2,3,4]. Magnetic resonance venography revealed non-visualizations of the deep venous system, superior sagittal sinus, straight sinus and bilateral transverse sinus normal. Lumbar puncture showed few lymphocytes with glucose: 98 mg% and protein: 36 mg%.
Endocrinology opined as transient peripartum DI (diabetes insipidus). Her endocrine work up for thyroid stimulating hormone and cortisol were all within normal limits. Urine osmolality was 190 mosm/L. On day three, a high vaginal swab culture was positive for ESBL Escherichia coli which was treated with a carbapenem. Over the next few days her metabolic parameters showed improving trends [Table1] and she was transferred to wards on seventh day. In the wards she developed an episode of folliculitis, which resolved with medications. Her left lower limb weakness improved gradually and she was discharged from the hospital on day 14, without any untoward events.
Discussion
Hypernatremia is a common electrolyte disturbance and is defined as a rise in serum sodium concentration to a value exceeding 145 mmol/L. The prevalence of hypernatremia in hospitalized patients has been reported to be between 0.2 and 1% [
1] and in ICU patients; the incidence is 2-52% [
2]. Multiple factors predispose to hypernatremia in ICU patients, including disturbed consciousness, sedation, severe brain injury, increased fluid loss (gastrointestinal, drainage fluids, open wounds, and insensible fluid loss due to fever or mechanical ventilation), the use of osmotic diuretics like mannitol to reduce intracranial pressure or the use of hypertonic and salt-containing fluids.
Gestational DI (GDI) identified more than 200 years ago is a rare phenomenon. The incidence is estimated between 2-6/100,000 pregnancies. It can occur at any stage of gestation and occasionally post-partum, but generally occurs at end of the second or third trimester of a first pregnancy. Diagnostic criteria for DI are urine osmolality >800 mosmol/kg water with concomitantly increased serum osmolality >295 mosmol/kg water or hypernatremia >145 mmol/L [
3,
4].
The pathogenesis of GDI are increased clearance of ADH due to increased levels of vasopressinase (nearly 1000 fold) produced by the syncytiotrophoblast of the human placenta; increased concentrations of corticosteroids, progesterone, and thyroxin, which antagonize ADH; reduced osmotic threshold for thirst perception [
6]. An increased production of renal prostaglandins (especially PGE2) during pregnancy can reduce renal sensitivity to ADH at the level of the renal tubules, resulting in an increase in polyuria in patients with partial DI of nephrogenic etiology [
7].
The clinical features might reveal a polyuric-polydypsic syndrome with fluid intake ranging from 3-20 L/day. Nocturnal polyuria may be a very common reason to consult a doctor. Clinical examination will be normal or may show disturbances in hydration in comatose patients due to inadequate water intake. Laboratory results are usually normal in GDI patients, but it is important to know that during pregnancy POsm decreases by almost 10 mmol/L and sodium concentration decreases by almost 5 mEq/L. Urine osmolality will be significantly reduced; nevertheless, fluid intake, urine output, plasma concentration of ADH, plasma osmolality and levels of sodium and glucose in blood and urine should be assessed in patients who have signs and symptoms suggestive of GDI. Cerebral scanning in patients with GDI show a loss of the hyper-signal in the posterior pituitary gland because of a decrease in vasopressin reserves [
8].
Our patient had a very high serum osmolality of 421 mosm/L, low urine osmolality, elevated CPK and was from a water scarce area with a dry climate where people are averse to drinking water. This was her first pregnancy and the initial investigations did resemble DI but the MRI showed high attenuation around the cerebral peduncles, midbrain, pons, thalamocapsular regions and splenium [Fig.3,4]. On our literature search we found one reference with a series of 11 cases reported from Northern Karnataka, which had MRI findings similar to our case [9] with elevated CPK. This case series reported a very high mortality though our patient recovered and was discharged home. We could not find any corroborative evidence to say that it is a unique syndrome until then it has to be accepted as a variance of DI.
Conclusion
Hypernatremia due to volume loss secondary to diuretics is a common event during hospital stay and more frequent in intensive care setting. If corrected expeditiously and cautiously can be very rewarding and yield an almost normal life.
References
- Palevsky PM, Bhagrath R, Greenberg A. Hypernatremia in hospitalized patients. Ann Intern Med. 1996;124:197-203.
- Lindner G, Funk GC, Schwarz C, Kneidinger N, Kaider A, Schneeweiss B, et al. Hypernatremia in the critically ill is an independent risk factor for mortality. Am J Kidney Dis. 2007;50:952-957.
- Bagshaw SM, Townsend DR, McDermid RC. Disorders of sodium and water balance in hospitalized patients. Can J Anaesth. 2009;56:151-167.
- Kumar S, Berl T. Sodium. Lancet. 1998;352:220-228.
- Tisdall M, Crocker M, Watkiss J, Smith M. Disturbances of sodium in critically ill adult neurologic patients: a clinical review. J Neurosurg Anesthesiol. 2006;18:57-63.
- Lindheimer MD, Davison JM. Osmoregulation, the secretion of arginine vasopressin and its metabolism during pregnancy. Eur J Endocrinol. 1995;132:133-143.
- Bernheim J, Shapira J, David F, Behari C, Gelerntner I, Rathaus M. Renal prostaglandins E2 and F2 alpha throughout normal human pregnancy. Eur J Clin Invest. 1986;16:113-116.
- Aleksandrov N, Audibert F, Bedard M, Mahone M, Goffinet F, Kadoch, I. Gestational Diabetes Insipidus: A Review of an Underdiagnosed Condition. Journal of Obstetrics and Gynaecology. 2010;32(3):225-231.
- Naik K, Saroja A. Seasonal postpartum hypernatremic encephalopathy with osmotic extrapontine myelinolysis and rhabdomyolysis. Journal of the Neurological Sciences. 2010;291(1-2):5-11.